The shortage stems from post-COVID workforce burnout, employer restrictions, and limited clinical sites across mental health settings. Most PMHNP students must secure their own preceptors to complete required clinical hours, but competition for qualified psychiatric providers has made placements harder to find and sustain — prompting many to seek structured support or preceptor matching services to stay on track.
TL;DR: Why It’s So Hard to Find PMHNP Preceptors (And What You Can Do About It)
- The PMHNP preceptor shortage is real and worsening.
Post-COVID burnout, employer restrictions, and limited clinical sites have made it harder than ever for PMHNP students to secure quality clinical rotations in mental health care. - Even “free” preceptors come with hidden costs.
Time, travel, paperwork, and uncertainty often turn the search into an exhausting process that delays graduation and drains motivation. - Systemic issues fuel the struggle.
From unclear affiliation agreements to productivity pressures on psychiatric providers, the placement process often fails both students and potential preceptors. - Students can take strategic steps to regain control.
Clear preparation, early networking, flexible site selection, and professionalism can dramatically improve your chances of finding the right preceptor and gaining meaningful clinical experience. - When the search stalls, trusted support makes all the difference.
Services like NPHub connect PMHNP students with verified psychiatric mental health preceptors, ensuring compliant placements, mentorship, and peace of mind — so you can focus on learning, not logistics.
The Growing Demand for PMHNPs and the Clinical Placement Shortage
Finding PMHNP preceptors has never been easy, but since COVID-19, it’s become one of the biggest roadblocks for nurse practitioner students. Clinical rotations are the backbone of every PMHNP program, yet the number of qualified preceptors and clinical sites hasn’t kept pace with the explosion in mental health needs across the country.
According to recent research, the preceptor shortage is long-standing and worsening, and the pandemic didn’t just interrupt placements temporarily, it reshaped how clinical training functions altogether.
Fear of exposure, lack of PPE, and redeployment of nurse practitioners meant many clinical sites simply stopped accepting students. Even after restrictions lifted, a new set of barriers remained, especially in mental health care and primary care settings where psychiatric mental health nurse practitioners (PMHNPs) are most needed.
The workforce itself has also shrunk. Burnout and low compensation compared to other specialties have driven many advanced practice nurses to reduce hours or leave clinical practice entirely.
Only about a third of NPs now work in primary care, which has sharply reduced the pool of qualified preceptors available to supervise students and support clinical learning experiences. Fewer practicing clinicians means fewer professionals who can guide students through psychiatric care, medication management, and behavioral health treatment plans in real-world settings.
Employers add another layer to the problem. Around 60% of nurse practitioners report not currently precepting, and over a third say it’s simply because no one asked. Meanwhile, nearly another third are restricted by their employer from accepting students due to productivity pressures or internal policy limits.
In fast-paced healthcare environments where every hour must be billable, teaching slows workflow, and for clinicians whose income depends on volume, mentoring can feel like a financial penalty.
This bottleneck creates a ripple effect throughout nurse practitioner programs. Schools now compete for the same limited number of potential clinical sites, often overloading willing preceptors with multiple students at once.
Large programs dominate the best urban placements, while smaller schools and students in rural or underserved areas are left waiting months for approval. The result is a system that’s unbalanced, inequitable, and exhausting for both students and faculty trying to secure qualified preceptors.
In short, this isn’t just about one student struggling to find a rotation, it’s a symptom of a national imbalance between how many mental health providers we need and how few we’re supporting to teach.
If you want a head start in navigating this reality, skip the cold calls and stalled email chains. Create your free NPHub account and search verified PMHNP preceptors who meet your school’s standards and are ready to provide real-world, supervised clinical experience.
In the meantime, in this blog, we’ll break down why the preceptor shortage persists, what research says could actually fix it, and how you can take control of your own placement process to keep your PMHNP journey on track.
Why Finding a PMHNP Preceptor Is So Challenging
Every PMHNP student knows the feeling of endless outreach emails, unreturned calls, and growing anxiety as deadlines close in. But the problem goes far beyond individual effort.
The difficulty in finding psychiatric mental health nurse practitioner (PMHNP) preceptors stems from a mix of systemic barriers, workforce burnout, and institutional disconnection that have only intensified since the pandemic.
At the root is a national workforce shortage. Across the country, nurse practitioners and primary care providers are leaving clinical practice or cutting back hours due to stress, burnout, and comparatively lower compensation.
As a result, the number of active clinicians willing to supervise students has declined sharply. This leaves nurse practitioner programs scrambling to find qualified preceptors who can provide the supervised clinical hours required for graduation and national certification.
Even those who remain in practice face growing employer restrictions. Research shows that about one-third of nurse practitioners are directly prohibited from precepting due to institutional policies designed to protect productivity.
Another 37% said they simply weren’t asked, a staggering oversight that reflects poor communication between academic programs and healthcare settings. It’s not that clinicians don’t want to teach; it’s that the system doesn’t make it easy or rewarding to do so.
If you’ve hit that wall yourself it’s not because you’re doing anything wrong. The process is broken and the reason why many PMHNP students turn to NPHub, where you can create a free account and move forward when traditional networking and placement systems fall short, giving you access to real clinical sites and mental health providers ready to teach.
These issues converge in a single outcome: intense competition for clinical sites. With fewer qualified preceptors, both large and small schools are vying for the same placements. Urban programs tend to dominate well-established psychiatric care networks, while students in rural or underserved areas are left with limited options or extended wait times.
Many programs rely on overburdened clinical coordinators who juggle hundreds of placement requests each term, leading to uneven opportunities and long approval delays.
Post-COVID realities have only magnified these gaps. During the height of the pandemic, many clinical sites closed their doors to students due to infection risks and PPE shortages. Years later, that ripple effect remains: some mental health providers never resumed precepting, and others reduced their patient loads to protect work–life balance.
The loss of those educators continues to strain the placement process, especially in high-demand specialties like psychiatry and behavioral health.
Ultimately, this is a structural imbalance between growing mental health needs and limited training capacity. The system relies on preceptors to train the next generation of psychiatric providers, yet offers them little time, support, or incentive to do so. Until that changes, students will continue facing the same uphill climb to meet their required clinical hours and build real-world clinical experience in mental health settings.
In the next section, we’ll look at how this imbalance affects not just students but the entire mental health workforce and what could actually make preceptorships sustainable again.
The Hidden Cost of “Free” PMHNP Clinical Rotations Search
On paper, finding your own PMHNP preceptors sounds simple, and best of all, free. But for most nurse practitioner students, what starts as a cost-saving decision quickly becomes one of the most draining parts of graduate school.
The reality is that “free” often means trading money for time, stress, and lost clinical experience, and sometimes, even delaying your entire PMHNP program.
Most PMHNP students spend 150 to 200 hours searching for a qualified preceptor who meets their school’s clinical placement requirements, aligns with their specialty, and is located within reach of their geographic location.
They cold-call community clinics, email mental health providers, and contact psychiatric care centers, hoping someone will accept students. But with limited potential clinical sites, it’s common to wait months before securing the right match.
And that delay can be devastating. Each lost week means postponed clinical rotations, fewer supervised hours, and more stress as you juggle coursework, work, and life responsibilities. Many NP students who pursue the DIY route end up extending their studies, paying for additional semesters, losing income, or delaying national certification.
What looked like a “free” process turns into a costly setback that impacts both your patient care experience and your future as a psychiatric mental health nurse.
The emotional toll is just as heavy. The endless follow-ups and unanswered messages chip away at confidence, making even motivated students question their path in psychiatric nursing. With clinical coordinators overwhelmed and behavioral health sites at capacity, you’re often left to navigate a maze of affiliation agreements, paperwork, and compliance steps alone.
That’s where rethinking your strategy makes sense. Services designed for PMHNP clinical placements help match you with qualified preceptors in real mental health settings who can offer hands-on clinical experience in areas like bipolar disorder, substance use, and psychiatric medication management. Create now your free account at NPHub and search a network of over 2,000 vetted preceptors in 10 different specialties who understand your goals and help you complete your clinical hours on time.
Next, we’ll look at what actually works to fix this system. from clearer role definitions to stronger academic–clinical partnerships that make preceptor placement more consistent, fair, and accessible for every student.
Breaking Through the PMHNP Preceptor Shortage: Real Solutions for Students
By now, you’ve probably realized that finding PMHNP preceptors isn’t just about persistence, it’s about navigating a system that’s stretched thin. Faculty burnout, restrictive employers, and shrinking clinical networks have made preceptor placement one of the hardest parts of becoming a psychiatric mental health nurse practitioner.
Even before the pandemic, nurse practitioner students struggled to find enough clinical sites to meet their required clinical hours. COVID-19 made it worse, forcing many experienced psychiatric providers out of teaching roles due to burnout and workload pressure.
Add employer restrictions and a growing number of NP programs competing for the same limited mental health settings, and the shortage becomes personal — delayed graduation, lost opportunities, and endless stress.
But while the system is flawed, you’re not powerless. Here’s how PMHNP students can take control of their clinical placement process, build confidence, and secure the kind of real-world experience that shapes exceptional future practitioners.
1. Start With Clarity and Intention
Before sending a single email, make sure you understand your PMHNP program inside and out. Review your required hours, acceptable clinical settings, and preceptor qualifications.
Know whether your school accepts psychiatric nurse practitioners, psychiatrists, or other mental health providers as supervisors.
Preceptors want to help, but they can’t read between vague requests. When you clearly communicate your program’s expectations and how your learning goals align with their clinical practice, you instantly stand out.
This is your first professional impression in the world of psychiatric mental health nursing, make it precise, confident, and respectful of their time.
2. Build Your Network Before You Need It
Most PMHNP students wait too long to start their search, often relying on last-minute outreach or overused hospital contacts. Instead, start early and think community-first.
Join your local chapter of the American Psychiatric Nurses Association (APNA) or your state’s nurse practitioner association. Attend mental health conferences, online meetups, or even volunteer at community behavioral health programs.
These connections often lead to potential preceptors who don’t advertise openings but are open to mentoring a motivated student. Don’t underestimate the power of word-of-mouth, many of the best clinical placements come from simple introductions or colleagues within your healthcare setting who can vouch for your professionalism and passion.
3. Lead With Professionalism and Gratitude
When a qualified preceptor agrees to take you on, treat it like the career opportunity it is. Show up early, prepare for every session, and always follow up on feedback. Small gestures like handwritten thank-you notes or offering to help with nonclinical tasks go a long way in building mutual respect.
Preceptors supervise students not for financial reward but because they care about shaping the next generation of mental health care providers.
Showing gratitude, initiative, and professionalism not only improves your learning experience but can also open doors to future collaborations, mentorship, or even job offers in psychiatric care.
4. Stay Open to Unexpected Opportunities
The “perfect” clinical site may not look the way you imagine. Many psychiatric mental health nurse practitioners began their careers in settings outside traditional hospitals — think rural clinics, substance use programs, correctional facilities, or community mental health centers.
These environments often provide richer exposure to psychiatric disorders, medication management, and complex treatment plans than larger institutions. They also give you a chance to support underserved populations while strengthening your diagnostic and therapeutic confidence.
Flexibility doesn’t mean settling, it means gaining hands-on experience that sets you apart when you take your national certification exam or apply for your first position in psychiatric mental health services.
Bonus: When You’ve Tried Everything, Simplify With Preceptor Matching Services
Sometimes, despite all your effort, the process stalls. Emails go unanswered, affiliation agreements take months, and deadlines loom. That’s where preceptor matching services can help bridge the gap between students and verified clinical mentors.
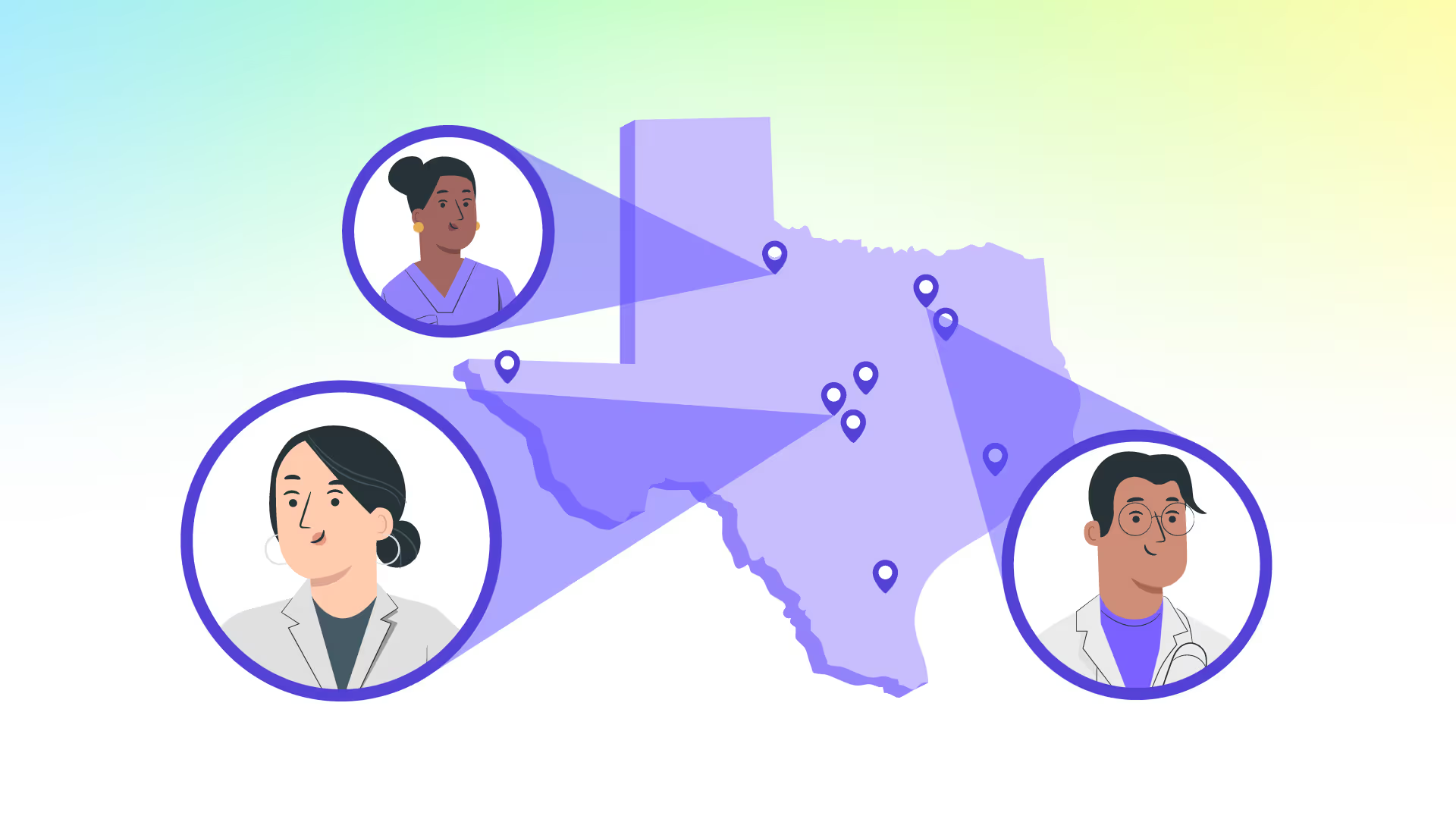
Platforms like NPHub were built specifically for PMHNP students who need access to vetted psychiatric preceptors in outpatient clinics, inpatient psychiatric facilities, or community mental health settings. You’ll still complete the same supervised hours and clinical training, but without the uncertainty, cold calls, or administrative back-and-forth that can delay your graduation.
When you create your free NPHub account, you gain access to a network of experienced psychiatric mental health nurse practitioners who are ready to teach, mentor, and guide you through a seamless, streamlined process that prioritizes both compliance and clinical growth.
It’s not a shortcut, it’s a smarter, more reliable way to keep your education on track and your career momentum strong.
Finding PMHNP preceptors shouldn’t feel like a full-time job, but until schools and employers fix the pipeline, students need strategies that work now.
Whether you network your way in or use a trusted matching platform, the goal remains the same: to gain the clinical experience that transforms you from student to confident provider.
Why NPHub Exists (and Why It’s Here for You)
If you’ve ever spent hours cold-emailing clinics, waiting on replies that never come, or watching your rotation deadlines creep closer while your inbox stays empty — you’re not alone.
We see it all the time: every semester, thousands of PMHNP students face the same wall: a broken clinical placement system that leaves them stressed, behind schedule, and questioning their path.
That’s exactly why NPHub was created. We connect NP students directly with verified psychiatric providers and mental health preceptors across the country, professionals who understand your program requirements and are ready to teach, mentor, and guide the next generation of mental health leaders.
When you create your free NPHub account, you’re not just finding a clinical site — you’re unlocking a streamlined, student-first system that handles the hardest parts for you:
- Verified, qualified preceptors in outpatient clinics, inpatient psychiatric facilities, and community mental health centers.
- A streamlined placement process that saves you from endless email loops and administrative hurdles.
- Personalized support from a team that actually understands PMHNP programs, clinical hours, and your deadlines.
Most importantly, you take back control. You stop waiting on chance and start building momentum toward your PMHNP certification and future clinical practice. Because your time should be spent treating patients and growing your skills, not refreshing your inbox.
From Student to Provider: Your Journey Starts Here
If you’ve made it this far, you already know something most people don’t, that becoming a psychiatric mental health nurse practitioner isn’t just about passing exams or checking off clinical hours.
It’s about persistence. It’s about grit. It’s about learning how to keep showing up for yourself and your future patients even when the system makes it unnecessarily hard.
Because it is hard. No one really prepares you for the countless unanswered emails, the polite rejections, or the slow anxiety that builds when deadlines creep closer and no qualified preceptor has said yes yet. You’re balancing coursework, jobs, families, sometimes all three, while trying to secure clinical placements that will determine your graduation date and your entire career path.
But here’s the truth that rarely gets said out loud: this process, frustrating as it is, is also shaping you into the kind of PMHNP the world desperately needs. The one who knows how to problem-solve under pressure. The one who doesn’t give up when the system says no. The one who understands what it feels like to fight for access, so later, when you’re the provider, you fight just as hard for your patients to access care.
Your clinical rotations are your first taste of what it means to lead. You’ll walk into each healthcare setting and you’ll start to see how your clinical expertise translates into impact. You’ll evaluate patients, manage treatment plans, recognize psychiatric symptoms, and learn to see the person behind the diagnosis.
And in between the stress and the exhaustion, there will be moments, real, quiet moments, where you realize you’re not just learning to provide mental health care; you’re learning to restore dignity, stability, and hope.
That’s what this journey is really about. It’s not just about meeting your required hours or finding the perfect preceptor. It’s about growing into someone who can hold space for pain, chaos, and recovery, someone who knows what it means to carry others through their darkest moments without losing compassion.
And yes, the path there is messy. Sometimes it feels unfair. But you don’t have to go through it alone. The truth is, finding your footing in this profession often starts with finding the right people, mentors who see your potential, preceptors who challenge and support you, and communities that believe in your purpose.
That’s exactly why NPHub exists, to give you a place to start, to help you stop spinning your wheels, and to make sure you never have to sacrifice your dreams because of broken logistics.
When you create your free NPHub account, you’re not just getting matched with a psychiatric provider, you're joining a network of people who’ve been where you are, who remember what it was like to be the student desperately trying to find their first chance to prove themselves.
So take that first step. Reach out. Keep trying. Keep believing that what you’re doing matters — because it does. Every email you send, every interview you schedule, every clinical hour you complete, it’s building the foundation of a career that saves lives and restores mental well-being in a world that needs it more than ever.
You’re not just becoming a psychiatric mental health nurse practitioner. You’re becoming the kind of provider who sees both the patient and the person. And it all starts here, with your courage, your persistence, and the first preceptor who says yes..
FAQ: Why It’s So Hard to Find PMHNP Preceptors (And What You Can Do About It)
1. Why is it so hard to find PMHNP preceptors?
It’s not your imagination — the shortage is real. Many psychiatric mental health providers have reduced clinical teaching due to burnout, workload pressure, and lack of institutional support. Post-COVID disruptions and restrictive employer policies have made clinical placements harder to secure, especially in mental health settings.
2. How do I find a qualified PMHNP preceptor for my clinical rotations?
Start with clarity. Know your program’s required clinical hours, approved clinical sites, and supervision criteria. Then, reach out to community mental health centers, behavioral health programs, or psychiatric outpatient clinics. If that feels overwhelming, you can simplify your search through preceptor matching services like NPHub, which connects PMHNP students with vetted psychiatric providers ready to teach.
3. Can I complete PMHNP clinical hours in non-traditional settings?
Absolutely. Your clinical experience doesn’t have to be limited to hospitals. Many nurse practitioner students complete rotations in correctional facilities, telepsychiatry, substance use programs, or community clinics. These sites often provide richer patient interactions and more autonomy, helping you gain real-world psychiatric care skills that strengthen your professional confidence.
4. What qualifications should my PMHNP preceptor have?
A qualified preceptor should be a licensed and board-certified Psychiatric-Mental Health Nurse Practitioner (PMHNP-BC), psychiatrist, or another licensed mental health provider authorized to supervise NP students. Always confirm their credentials and your school’s preceptor eligibility rules before your clinical rotation begins.
5. How early should I start searching for a PMHNP preceptor?
The earlier, the better. Begin your search at least six months before your rotation starts. Many nursing programs require affiliation agreements or background checks that can delay site approval. Starting early gives you time to explore multiple potential preceptors, avoid rushed decisions, and stay on track for graduation.
6. Are preceptor matching services worth it?
For many students, yes. If you’ve already reached out to local mental health clinics and hospitals with no luck, preceptor matching services like NPHub can save you time and frustration. They help you connect with verified psychiatric providers, streamline paperwork, and ensure your clinical placements meet your program’s standards — no cold calls, no guesswork.
7. Can my employer or current clinical site count toward my PMHNP hours?
In some cases, yes. If your employer offers psychiatric or behavioral health services, and there’s a qualified preceptor available, you may be able to complete supervised hours there. Just make sure your clinical coordinator approves the site to avoid conflicts of interest.
8. Do PMHNP students get paid for clinical rotations?
No — your clinical rotations are part of your PMHNP program’s educational requirements, not paid employment. However, some employers offer educational leave or tuition assistance, especially in rural or underserved areas where they want to retain skilled psychiatric nurse practitioners after graduation.
9. What happens if I can’t find a preceptor before my rotation deadline?
Don’t panic, but act fast. Notify your program director or clinical coordinator immediately — some schools have backup partnerships or can grant temporary extensions. If traditional outreach doesn’t work, consider trusted matching services like NPHub to secure your clinical placement quickly and keep your graduation timeline intact.
10. How can I make a strong impression once I find a preceptor?
Treat your clinical rotation like the start of your career. Be early, prepared, and proactive. Ask thoughtful questions, take feedback seriously, and always express gratitude. Great preceptors notice professionalism and commitment — and those relationships can turn into mentorship, job references, or future opportunities in psychiatric mental health care.
Key Definitions for PMHNP Students
- PMHNP (Psychiatric-Mental Health Nurse Practitioner)
An advanced practice registered nurse (APRN) trained to assess, diagnose, and treat individuals with mental health disorders. PMHNPs provide therapy, prescribe medications, and manage treatment plans in various healthcare settings. - Clinical Rotations
Supervised, hands-on training experiences required in all nurse practitioner programs. PMHNP students complete rotations in approved clinical sites such as outpatient clinics, behavioral health centers, and psychiatric hospitals to gain real-world clinical experience. - Preceptor
A licensed healthcare professional — usually a PMHNP-BC or psychiatrist — who supervises, mentors, and evaluates students during their clinical placements. Preceptors help students bridge classroom knowledge with real-world patient care. - Clinical Hours
The total number of supervised hours a nurse practitioner student must complete in clinical settings to meet graduation and certification requirements. Most PMHNP programs require between 500 and 700 hours of direct clinical practice. - Clinical Site
An approved healthcare setting where NP students complete their rotations. Common mental health settings include outpatient psychiatric clinics, community mental health centers, correctional facilities, and inpatient psychiatric units. - Affiliation Agreement
A formal contract between a nursing school and a clinical site that authorizes students to complete rotations there. This agreement ensures liability coverage, supervision standards, and compliance with academic policies. - National Certification (PMHNP-BC)
A credential earned after completing a PMHNP program and passing the ANCC Psychiatric-Mental Health Nurse Practitioner certification exam. It verifies clinical competency in diagnosing and treating psychiatric disorders.
About the author
- NPHub Staff
At NPHub, we live and breathe clinical placements. Our team is made up of nurse practitioners, clinical coordinators, placement advisors, and former students who’ve been through the process themselves. We work directly with NP students across the country to help them secure high-quality preceptorships and graduate on time with confidence. - Last updated
October 7, 2025 - Fact-checked by
NPHub Clinical Placement Experts & Student Support Team - Sources and references
Find a preceptor who cares with NPHub
Book a rotation.webp)







.webp)


.webp)


%20(3)%20(2).svg)
.webp)