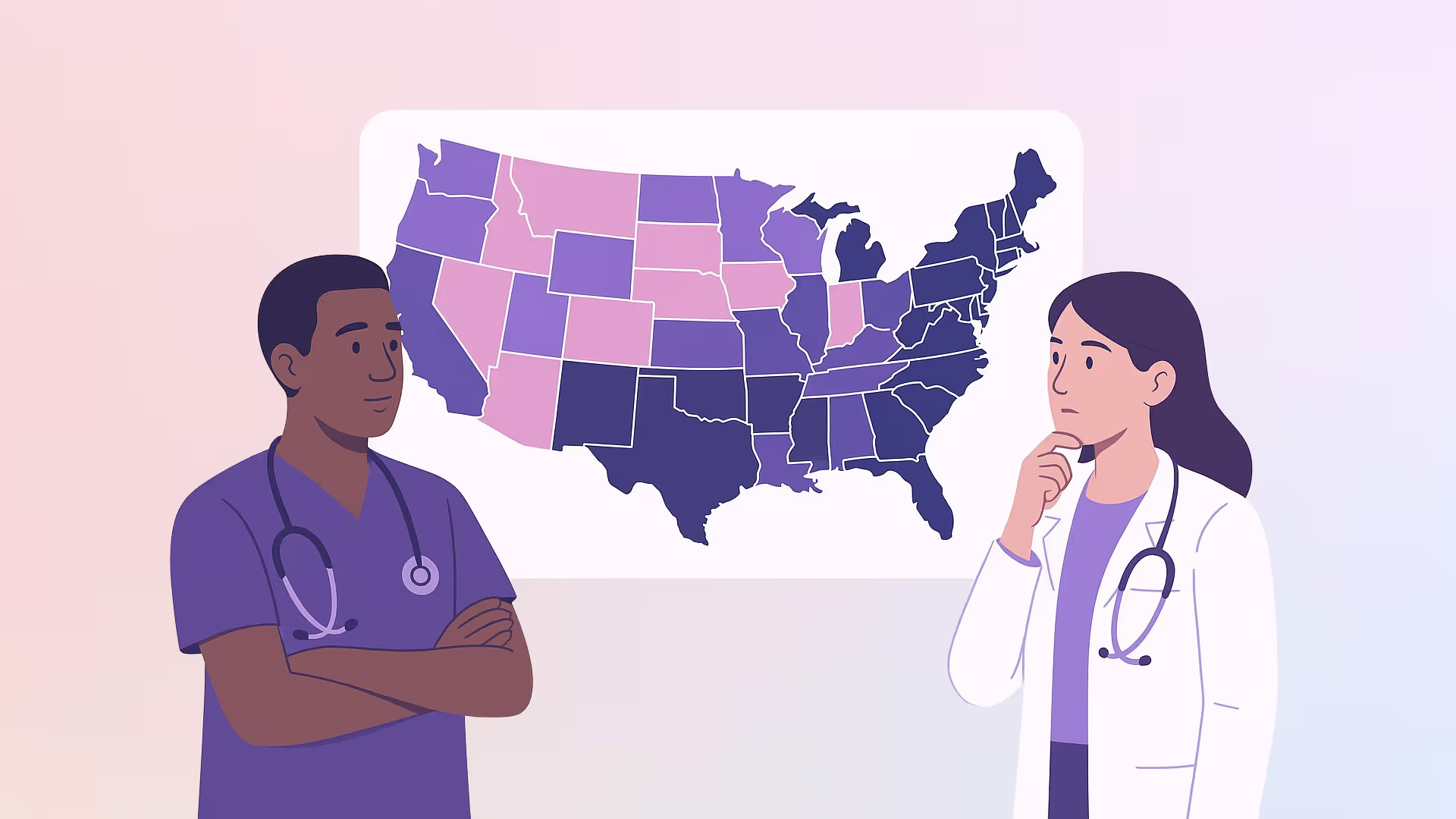
Nurse Practitioner Scope of Practice: State NP Clinical Requirements Comparison Guide
State NP clinical requirements define what nurse practitioners can legally do in each state, including diagnosing conditions, interpreting diagnostic tests, prescribing medications, and delivering patient care. These requirements—based on state scope of practice laws—determine whether an NP must work under physician supervision, follow a collaborative agreement, or can practice independently with full authority.
TL;DR: What You Need to Know About NP Scope of Practice by State
- NP practice laws vary by state, determining whether you can work independently or need physician supervision.
- There are 3 authority levels: full (independent), reduced (collaborative agreement), and restricted (direct supervision).
- Licensure alone isn’t enough—some states require extra supervised hours or transition periods before granting autonomy.
- Scope of practice affects your day-to-day: from prescribing meds to launching your own practice.
- Knowing your state’s rules is essential for planning your career, choosing preceptors, and delivering care with confidence.
Why State NP Clinical Requirements Matter More Than Ever?
Whether you're fresh out of your NP program or a seasoned provider eyeing a better practice setting, understanding your state's clinical requirements is non-negotiable.
These rules dictate everything from how you manage treatments and interpret diagnostic tests to whether you can prescribe medications or need a physician’s signature to sneeze.
The catch? Not all states treat nurse practitioners equally. Some grant full practice authority, letting NPs run independent practices and deliver cost-effective, high-quality health care. Others still cling to outdated restrictions, requiring reduced or restricted practice authority, where physician involvement and collaborative agreements are baked into every chart and prescription pad.
This guide compares the current state practice environments across the U.S. so you can plan your career, avoid surprises, and confidently practice to the full extent of your training.
Understanding Nurse Practitioner Scope of Practice
“Nurse practitioner scope of practice” refers to the legal boundaries that define what nurse practitioners (NPs) can and cannot do clinically and it’s far from one-size-fits-all.
While some NPs practice as independent practitioners, others are legally tethered to physician supervision or collaborative agreements based on their state's regulatory model.
At its core, scope of practice defines whether and how NPs can:
- Diagnose and treat patients across primary care, acute care, and mental health settings
- Interpret diagnostic tests like labs and imaging
- Prescribe medications, including controlled substances
- Manage chronic diseases and implement evidence-based treatment plans
- Deliver public health and preventive care independently or in collaboration
Scope of practice is established by state practice laws and enforced by each state board of nursing or medicine. These laws apply to all advanced practice registered nurses (APRNs), including those with population foci such as family (FNP), adult-gerontology (AGNP), or psychiatric mental health (PMHNP)
And here’s the real kicker: just because you’re certified and licensed doesn’t mean you’ll get to use the full extent of your skills in every state. That’s why understanding your NP scope of practice is one of the most important factors when evaluating your practice setting, relocation plans, or professional license path.
State NP Clinical Requirements: Licensure, Certification, and Supervision
The clinical authority granted to nurse practitioners begins long before they enter a patient room, it starts with fulfilling the educational, licensure, and legal obligations set by each individual state.
These requirements determine not just whether you can practice, but how much of your training and clinical expertise you’re actually allowed to use.
While all states recognize nurse practitioners as advanced practice registered nurses (APRNs), not all states authorize them to practice independently.
Clinical requirements differ depending on the state’s stance on practice authority, which falls into three general categories: full, reduced, or restricted practice. To navigate this system effectively, it’s essential to understand what each state expects from an NP before, during, and after initial licensure.
Education and National Certification
Every NP must begin with the same foundation: completing an accredited graduate nursing program, typically a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP). These programs focus on population foci, such as Family (FNP), Adult-Gerontology (AGNP), Pediatric (PNP), Women’s Health (WHNP), or Psychiatric-Mental Health (PMHNP)
Upon completing the educational requirements, nurse practitioners are required to pass a national certification exam from one of two major organizations:
- The American Academy of Nurse Practitioners Certification Board (AANPCB): certifies NPs in family and adult-gerontology primary care.
- The American Nurses Credentialing Center (ANCC): offers certification in multiple specialties, including psychiatric-mental health and acute care [AANP, 2024].
These certifications validate clinical competency in assessment, diagnosis, treatment planning, prescribing, and management of acute and chronic conditions. However, certification alone does not grant full authority to practice, that decision lies with each state.
State Licensure: Professional License vs. Practice Limitations
After obtaining national certification, NPs must apply for licensure through their respective state board of nursing (or, in some cases, a joint medical board).
The requirements for this professional license vary greatly from state to state and often reflect the scope of practice and practice authority level defined in state law, for example:
- In full practice authority states, the licensure process is typically straightforward: submit proof of education, certification, and a background check, and you’re authorized to treat patients, prescribe medications, and interpret diagnostic tests without physician involvement.
- In reduced practice authority states, licensure may require proof of a collaborative agreement with a physician, limiting how and where NPs can deliver medical care.
- In restricted practice authority states, nurse practitioners often need ongoing documentation of physician supervision, co-signed charts, or even on-site oversight for certain services like prescribing or diagnostic testing.
In many reduced or restricted states, licensure is not considered “active” for full practice until collaborative agreements are in place even if the NP is fully certified and credentialed.
Physician Supervision, Collaborative Agreements, and Transitional Practice Periods
This is where state NP clinical requirements really start to diverge. In reduced and restricted practice states, NPs may be legally obligated to:
- Maintain a collaborative agreement with a physician that specifies the scope of tasks they are allowed to perform.
- Undergo peer review, often involving regular performance evaluations, documentation audits, or chart sign-offs.
- Have a supervising physician physically present or immediately available, depending on the state’s interpretation of “supervision”.
- Practice under supervision for a specified period (e.g., 2,000 clinical hours or 3 years) before applying for independent practice status—if the state even allows it.
Some states, like California and Alabama, impose specific restrictions related to prescribing controlled substances or interpreting diagnostic tests, requiring additional training, oversight, or time under supervision.
Additionally, certain states have begun temporarily suspending collaborative agreement requirements to address physician shortages or expand access to care during public health emergencies, though these suspensions may not be permanent.
In summary, understanding your state’s licensure process isn’t just a box to check, it directly shapes the limits of your NP scope of practice.
The combination of certification, licensure, and supervision determines whether you’ll be practicing as an independent practitioner in a full practice authority state or whether your day-to-day patient care will be governed by practice barriers like physician collaboration, regulatory oversight, or reduced prescriptive authority.
Once you understand what’s required to become a licensed nurse practitioner in your state, the next critical step is knowing what that license actually allows you to do.
That’s where the NP scope of practice categories, full, reduced, and restricted, come into play. Let’s break down what each level means for your clinical freedom, day-to-day responsibilities, and your ability to provide quality health care.
NP Scope of Practice: Full vs Reduced vs Restricted Practice
Once you’re licensed and certified, the next question is: what exactly are you allowed to do? That’s where the concept of NP scope of practice comes into sharp focus.
In the U.S., nurse practitioners operate under one of three legally defined practice authority categories: full, reduced, or restricted. These categories dictate the degree of clinical autonomy you have, affecting everything from how you treat patients to whether you need physician involvement to order diagnostic tests or prescribe medications.
Full Practice Authority
Nurse practitioners in full practice authority states are allowed to:
- Diagnose and treat patients independently
- Interpret diagnostic tests
- Prescribe medications, including controlled substances
- Establish independent practices and follow their own practice guidelines
States with full practice authority recognize NPs as primary care providers who can deliver quality health care without physician supervision or a collaborative agreement. As of 2025, there are 27 such states, plus the District of Columbia.
These states allow NPs to practice to the full extent of their training and licensure immediately or after a short transitional period. Examples include New Hampshire, Rhode Island, North Dakota, Utah, and Washington.
Reduced Practice Authority
In states with reduced practice authority, NPs can still evaluate and manage patients but must maintain a collaborative agreement with a physician for at least one element of their practice.
Typical restrictions include:
- Limits on prescriptive authority (especially for controlled substances)
- Requirement for physician approval for certain diagnostic tests or treatment plans
- Mandated review of a percentage of patient charts through peer review systems
These states recognize NPs as key providers in health care, but legal barriers often prevent them from fully functioning as independent practitioners. The exact limitations vary significantly from state to state.
Restricted Practice Authority
In restricted practice authority states, NPs are required to practice under direct physician supervision for most, if not all, clinical tasks. This often includes:
- Direct oversight for prescribing medications
- Supervision while managing chronic diseases
- Physician sign-off on diagnostic testing
- Limits on practicing in solo or remote settings
Restricted states impose the most substantial practice barriers, frequently impacting patient access, particularly in underserved areas where physician shortages are most acute.
Now that you understand the key differences between full, reduced, and restricted NP practice authority, let’s take a closer look at how this plays out across the country. The next section offers a state-by-state comparison, so you can see exactly where your skills and autonomy are fully recognized and where legal restrictions still apply.
NP Practice Authority by State: A Comparison Guide
While NP scope of practice definitions give us the big picture, the real-world impact happens at the state level. Each U.S. state and the District of Columbia sets its own rules for how nurse practitioners can work, resulting in dramatically different practice environments across the country.
Whether you’re choosing where to apply, considering relocation, or just want to know where you can actually use your full skill set, this guide breaks it down clearly. Below, we summarize how practice authority, prescriptive rights, and collaborative requirements vary by state.
- Alabama
- Physician Involvement: Yes – A collaborative practice agreement (CPA) is required. Physicians must provide oversight, be accessible via communication, and be physically present at least 10% of the NP's scheduled hours.
- Supervised Hours: Not specified.
- The physician must visit the NP’s site quarterly. CPAs must also define protocols, consultation availability, emergency procedures, and quality assurance indicators, including review of at least 10% of medical records.
- Alaska
- Physician Involvement: No – Independent practice allowed.
- Supervised Hours: None.
- NPs must submit a written consultation and referral plan when delivering healthcare services. The plan must include procedures for routine referrals and quality assurance evaluations.
- Arizona
- Physician Involvement: No – Not required for general practice.
- Supervised Hours: None.
- NPs are expected to refer to physicians or healthcare providers if a patient's condition exceeds their training or scope. Monthly consultations are encouraged for quality care assurance.
- Arkansas
- Physician Involvement: Yes – Required for NPs and APRNs under collaborative agreements.
- Supervised Hours: Not applicable (N/A).
- CPAs must outline treatment guidelines, prescribing authority, and consultation availability. APRNs must meet specific education and licensing standards set by the board.
- California
- Physician Involvement: Yes – Required under "standardized procedures" jointly developed by physicians and healthcare administrators.
- Supervised Hours: Not specified.
- NPs can perform medical functions like prescribing and diagnosing only under standardized protocols, which must be collaboratively developed and reviewed.
- Colorado
- Physician Involvement: No – Full independent authority granted.
- Supervised Hours: None.
- NPs may sign off on various legal and medical documents, including advance directives and disability certifications, as long as they are recognized as RXN by the state Board of Nursing.
- Connecticut
- Physician Involvement: Yes – Required for the first 3 years and at least 2,000 hours of practice.
- Supervised Hours: 3 years and 2,000 hours minimum.
- The CPA must outline prescriptive scope, methods of physician collaboration, and a quality review process for patient outcomes. After completion, NPs may practice independently.
- Delaware
- Physician Involvement: Yes – Required for the first 2 years or 4,000 hours.
- Supervised Hours: 2 years and 4,000 hours.
- NPs may seek independent practice approval from a joint board after completing supervised time. Practice must align with the NP’s population focus and certification.
- District of Columbia (D.C.)
- Physician Involvement: No – Independent practice is granted at licensure.
- Supervised Hours: None.
- NPs are certified to practice fully and independently as long as their credentials meet DC standards.
- Florida
- Physician Involvement: Yes – General supervision is required for all practice under a written protocol.
- Supervised Hours: None.
- Physicians must specify their supervisory role and limits in a protocol. Certain specialties (e.g., plastic surgery or dermatology) have extra restrictions on NP locations and supervisory ratios.
- Georgia
- Physician Involvement: Yes – General supervision and delegation are required through a protocol agreement with a physician.
- Supervised Hours: Not specified.
- The protocol must include delegated acts, consultation procedures, refill and radiology restrictions, and chart review if prescribing controlled substances. NPs are not permitted to employ physicians to satisfy these requirements.
- Hawaii
- Physician Involvement: No – Independent practice is permitted.
- Supervised Hours: None.
- NPs must meet national certification and state licensure standards. They are authorized to sign death certificates and perform other functions independently.
- Idaho
- Physician Involvement: No – Independent practice allowed.
- Supervised Hours: None.
- NPs may diagnose, treat, and prescribe without collaborative agreements, including certifying disability parking and participating in workers’ compensation programs.
- Illinois
- Physician Involvement: Yes – A collaborative agreement is required unless practicing in a hospital or ambulatory surgical center.
- Supervised Hours: None.
- Monthly collaboration with a physician is required, which can be conducted remotely. The agreement must outline scope of services and consultation expectations.
- Indiana
- Physician Involvement: Yes – A collaborative agreement is required for all NP practice.
- Supervised Hours: Not specified.
- The agreement must describe coordination of care, and NPs are not allowed to enter agreements with physician assistants. NPs may order occupational therapy and authorize handicapped parking.
- Iowa
- Physician Involvement: No – Independent practice permitted.
- Supervised Hours: None.
- NPs must be nationally certified. They may sign death certificates, manage treatments, and prescribe independently in both primary and acute care settings.
- Kansas
- Physician Involvement: Yes – A collaborative practice agreement is required.
- Supervised Hours: Not specified.
- Written authorization must be signed by both the NP and the physician. NPs are accountable for independent judgment within the agreed scope.
- Kentucky
- Physician Involvement: No – Only required when practicing outside the NP’s certified role.
- Supervised Hours: None.
- NPs may independently treat patients, prescribe medications, and certify death or CDL eligibility within their certified population foci.
- Louisiana
- Physician Involvement: Yes – A collaborative agreement is required.
- Supervised Hours: 24 months.
- The agreement must define physician availability, clinical responsibilities, and patient care coordination. The initial 24 months must include documented oversight before autonomy is permitted.
- Maine
- Physician Involvement: Yes – Required for the first 24 months of NP practice.
- Supervised Hours: 24 months.
- Supervision may be provided by a physician or an NP in the same specialty who meets board criteria, including prior supervision, clinical experience, and board approval.
- Maryland
- Physician Involvement: Yes – Required for the first 18 months of practice. NPs must consult and collaborate with a physician or NP during this period.
- Supervised Hours: None.
- NPs may sign death certificates, issue DNRs, verify underage marriages, and certify births in hospitals. Additional procedures require documentation of training and competency after the NP program.
- Massachusetts
- Physician Involvement: Yes – Required via written practice guidelines.
- Supervised Hours: Not specified.
- Guidelines must describe NP scope, when physician consultation is needed, and protocols for managing common and emergency conditions.
- Michigan
- Physician Involvement: No.
- Supervised Hours: None.
- NPs may perform state-mandated physical exams but no additional supervisory protocols apply.
- Minnesota
- Physician Involvement: Yes – Required only for the first 2,080 hours.
- Supervised Hours: 2,080 hours.
- Collaborative agreement must define scope and care responsibilities between NP and physician/APRN. Afterward, independent practice is allowed.
- Mississippi
- Physician Involvement: Yes – A collaborative practice agreement is required.
- Supervised Hours: Not specified.
- Agreements must include chart reviews, log maintenance, and quarterly face-to-face meetings. Physicians cannot collaborate with NPs >75 miles away.
- Missouri
- Physician Involvement: Yes – Required via a collaborative practice agreement.
- Supervised Hours: Not specified.
- Physicians must be available for consultation at all times and review NP work biweekly. Distance rules apply for rural or shortage areas.
- Montana
- Physician Involvement: No.
- Supervised Hours: None.
- NPs may independently assess, diagnose, and manage patient care without a collaborative agreement.
- Nebraska
- Physician Involvement: Yes – Required only for the first 2,000 hours.
- Supervised Hours: 2,000 hours.
- Transition-to-practice agreements must be in writing, with defined scopes and joint management of care. Supervisors must meet specific experience and approval criteria.
- Nevada
- Physician Involvement: No.
- Supervised Hours: None (except controlled substance prescribing has separate conditions).
- NPs practice independently within their certified specialty.
- New Hampshire
- Physician Involvement: No.
- Supervised Hours: None.
- NPs are fully autonomous at the time of licensure and may practice without collaborative oversight.
- New Jersey
- Physician Involvement: No – NPs do not require physician collaboration for practice
- Supervised Hours: Not required.
- NPs may determine cause of death and certify it only when they are the patient’s primary caregiver.
- New Mexico
- Physician Involvement: No – Full independent practice.
- Supervised Hours: Not required.
- NPs can sign death certificates and certify disability for handicap parking passes without physician oversight.
- New York
- Physician Involvement: Yes – A collaborative practice agreement is required unless the NP has over 3,600 hours of experience.
- Supervised Hours: 3,600 hours required to be exempt from written agreement.
- NPs may write home health orders, declare emergencies under CLIA, and prescribe under specific conditions like HIV or TB treatment.
- North Carolina
- Physician Involvement: Yes – Collaborative agreement required.
- Supervised Hours: Monthly meetings first 6 months, then at least every 6 months.
- NPs must sign a protocol with a physician, including emergency plans and quality improvement plans, maintained at each practice site.
- North Dakota
- Physician Involvement: No – NPs can practice independently.
- Supervised Hours: None required.
- NPs can diagnose, treat, prescribe, and manage patient care without any physician involvement.
- Ohio
- Physician Involvement: Yes – Must enter a “standard care arrangement” with a physician or podiatrist.
- Supervised Hours: Not required.
- The agreement outlines services, prescriptive authority, and scope; NPs also have hospital admitting privileges.
- Oklahoma
- Physician Involvement: No – Independent practice allowed.
- Supervised Hours: None required.
- NPs can diagnose, treat, and prescribe medications without needing a formal collaborative agreement.
- Oregon
- Physician Involvement: No – Full practice authority.
- Supervised Hours: Required only for reentry.
- NPs can assess, diagnose, prescribe, and manage patients without restriction, including controlled substances.
- Pennsylvania
- Physician Involvement: Yes – Collaborative agreement required.
- Supervised Hours: Not specified.
- Agreement must include physician availability, referral protocols, and periodic chart reviews to maintain shared accountability.
- Rhode Island
- Physician Involvement: No – Independent practice is allowed.
- Supervised Hours: Not required.
- NPs are recognized as primary care providers and can assess, diagnose, prescribe, and manage patients autonomously in all settings.
- South Carolina
- Physician Involvement: Yes – General supervision and a practice protocol with a physician are required.
- Supervised Hours: Not specified.
- NPs can perform delegated medical acts under protocol but must maintain physician involvement throughout practice.
- South Dakota
- Physician Involvement: No – Independent practice allowed after meeting transition requirements.
- Supervised Hours: 1,040 hours of collaborative practice required for autonomy.
- After completion, NPs have full prescriptive authority and no requirement for a written agreement.
- Tennessee
- Physician Involvement: Yes – Supervision required for diagnosis and treatment.
- Supervised Hours: Not specified.
- A written protocol is required, and physicians must be available for consultation at all times during NP practice.
- Texas
- Physician Involvement: Yes – Delegation agreement required.
- Supervised Hours: Not specified.
• NPs must have a written prescriptive delegation agreement; physicians may oversee up to 7 NPs or PAs at once.
- Utah
- Physician Involvement: No – Full independent practice.
- Supervised Hours: 2,000 hours or 3 years of experience required to prescribe controlled substances independently.
- After this threshold, NPs have full authority to diagnose, treat, and prescribe, including controlled substances.
- Vermont
- Physician Involvement: No – Independent practice allowed.
- Supervised Hours: 2,400 hours and 24 months of mentored practice required.
- Once completed, NPs can practice and prescribe independently without any physician agreement.
- Virginia
- Physician Involvement: Yes – Collaboration required unless NP qualifies for autonomous practice.
- Supervised Hours: 9,000 hours (5 years) required for autonomy.
- Until then, NPs must maintain a practice agreement with a licensed physician or podiatrist.
- Washington
- Physician Involvement: No – NPs have full practice authority.
- Supervised Hours: Not required.
- NPs can assess, diagnose, treat, and prescribe independently, including controlled substances.
- West Virginia
- Physician Involvement: Yes – Initial collaboration required.
- Supervised Hours: 3 years (36 months) of collaboration needed for autonomy.
- After that, NPs can apply for independent practice and full prescriptive authority.
- Wisconsin
- Physician Involvement: Yes – Required for prescribing privileges.
- Supervised Hours: Not specified.
- NPs must collaborate with a physician to prescribe but may provide care independently otherwise.
- Wyoming
- Physician Involvement: No – NPs practice independently.
- Supervised Hours: None required.
- NPs can diagnose, treat, and prescribe, including controlled substances, with no mandated physician oversight.
How State NP Clinical Requirements Impact Patient Care and NP Careers
The patchwork of nurse practitioner scope of practice laws across the U.S. doesn’t just shape legal boundaries—it shapes real careers and patient outcomes.
Whether you’re an NP seeking independence or a student preparing for graduation, the regulatory environment of your state can drastically affect your clinical freedom, earning potential, and impact on the communities you serve.
Patient Access and Health Equity
In full practice authority states, patients often benefit from faster access to primary care and mental health services, particularly in rural or underserved areas.
NPs in these states can manage chronic diseases, prescribe medications, and deliver holistic care without waiting on physician approval—reducing delays and improving continuity of care.
Conversely, in restricted practice states, NPs often face barriers that limit their ability to respond to patient needs promptly. Requiring physician supervision can slow down routine treatments, limit telehealth access, and contribute to provider shortages, especially during health crises.
Career Opportunities and Autonomy
The state practice environment directly influences NP job satisfaction and professional mobility. In full authority states, NPs can launch their own independent practices, negotiate better contracts, and shape their roles based on patient needs rather than bureaucratic limitations.
However, in reduced or restricted states, career progression often hits a ceiling. From limitations on prescribing controlled substances to mandatory peer review systems, many NPs find themselves legally tethered—even after years of education, certification, and successful clinical experience.
The Reality for New NP Grads
If you’re just starting out, state regulations will dictate more than just your first job. They’ll determine how quickly you can practice independently, how long you must remain under supervision, and whether you’ll need a collaborative agreement to treat patients at all.
For some new grads, this can mean delayed career starts or being locked out of desired roles in telemedicine, urgent care, or rural health.
Know the Rules, Empower Your Practice
Navigating the legal maze of nurse practitioner scope of practice isn't just about ticking boxes—it’s about protecting your license, maximizing your autonomy, and delivering the best possible care to your patients.
Whether you’re mapping out your first clinical rotation or preparing to relocate, understanding state NP clinical requirements is key to avoiding delays, denials, or missed opportunities.
The more informed you are about your state’s licensing rules, physician involvement mandates, and transitional practice periods, the more control you have over your career trajectory.
That's why at NPHub, we help nurse practitioner students secure their clinical rotations in all 50 states, and that includes helping them understand where and how they’re legally allowed to practice.
From matching you with preceptors who meet your state’s and school requirements to giving you clarity around practice environments, our job is to make sure your clinical journey starts on solid ground.
Your future patients need a confident, well-prepared provider. And that starts with you knowing exactly what your state requires and where your scope of practice can truly thrive.
Frequently Asked Questions: Understanding Nurse Practitioner Scope of Practice and State NP Clinical Requirements
1. What is nurse practitioner scope of practice?
It refers to the range of medical care services NPs are legally authorized to perform in a given state—like diagnosing patients, interpreting diagnostic tests, prescribing medications, and managing treatments.
2. Which states allow full practice authority for nurse practitioners?
States like New Hampshire, Rhode Island, and North Dakota grant full practice authority, meaning NPs can treat patients, prescribe, and manage care without physician supervision.
3. What’s the difference between reduced and restricted practice authority?
Reduced practice requires a collaborative agreement for at least one element of care. Restricted practice demands direct physician supervision for most or all clinical tasks.
4. Can nurse practitioners prescribe medications in all states?
Yes, but with varying limits. Some states require a supervising physician for controlled substances or restrict which schedules an NP can prescribe.
5. What are the typical NP licensing requirements by state?
Most states require an MSN or DNP, national certification, and additional state-specific requirements like collaborative agreements or a supervised practice period.
6. What is the APRN Consensus Model?
It’s a national framework aimed at standardizing how NPs are licensed, certified, and allowed to practice across all states.
7. Do all states require a collaborative agreement for NPs?
No. Full practice states waive that requirement entirely. In reduced and restricted states, it’s still legally mandated to begin or maintain NP practice.
8. How do state regulations affect new NP graduates?
Many states require new grads to complete a transitional period—often 2,000 hours or more—before they can practice independently.
9. Is it worth relocating to a full practice authority state?
Absolutely—NPs in full authority states often enjoy higher job flexibility, less red tape, and greater autonomy in patient care.
10. What happens when a state changes its scope of practice laws?
NPs may gain or lose autonomy. Always stay up-to-date via your state board or organizations like the American Association of Nurse Practitioners (AANP).
Key Definitions: Know the Terms That Define Your Practice
Here’s a quick glossary of essential terms that every nurse practitioner should understand when evaluating state requirements and clinical authority:
- Scope of Practice
The range of medical services NPs are legally allowed to perform under state law. - Full Practice Authority
NPs can evaluate, diagnose, treat, and prescribe independently without physician oversight. - Reduced Practice
NPs must collaborate with a physician on at least one element of patient care. - Restricted Practice
NPs are required to work under physician supervision for most aspects of care. - Collaborative Agreement
A formal written agreement with a physician outlining shared roles, responsibilities, and oversight requirements. - Transitional Period
A required timeframe (e.g., 2,000 hours or 2 years) of supervised practice before gaining independence. - Prescriptive Authority
The legal right to prescribe medications, including controlled substances, which varies by state. - Population Foci
NP specialization areas such as family (FNP), adult-gero (AGNP), or psych-mental health (PMHNP). - APRN Consensus Model
A national framework aiming to standardize NP licensure, education, and scope of practice across states.
About the author
- NPHub Staff
At NPHub, we live and breathe clinical placements. Our team is made up of nurse practitioners, clinical coordinators, placement advisors, and former students who’ve been through the process themselves. We work directly with NP students across the country to help them secure high-quality preceptorships and graduate on time with confidence. - Last updated
Jun 16, 2025 - Fact-checked by
NPHub Clinical Placement Experts & Student Support Team - Sources and references
- https://www.ncsbn.org/exams.page
- https://www.aanp.org/student-resources
- https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/specialty%20group/arc/ama-chart-np-practice-authority.pdf
- https://www.bartonassociates.com/locum-tenens-resources/nurse-practitioner-scope-of-practice-laws/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9534177/pdf/nihms-1820683.pdf
Find a preceptor who cares with NPHub
Book a rotation.webp)







.webp)

.webp)


%20(3)%20(2).svg)
.webp)