Inpatient psychiatry clinicals are hospital-based rotations where PMHNP students gain hands-on experience caring for patients in acute mental health crises. Under the supervision of qualified preceptors, students participate in psychiatric assessments, medication management, crisis stabilization, and interdisciplinary teamwork. These rotations are a required part of most nurse practitioner programs, preparing students for national certification and future practice in high-acuity mental health settings.
TL;DR – PMHNP Clinicals in Inpatient Psychiatry
- Inpatient psychiatry clinicals give PMHNP students hands-on training in hospital-based settings, focusing on acute mental health care and crisis stabilization.
- During these rotations, students gain experience in psychiatric assessments, medication management, interdisciplinary teamwork, and discharge planning.
- Unlike outpatient rotations, inpatient units expose students to high-acuity psychiatric conditions like suicidal ideation, psychosis, bipolar disorder, and severe depression.
- Finding an inpatient psychiatry preceptor on your own is difficult—credentialing, paperwork, and limited clinical sites make the DIY process stressful and uncertain.
- NPHub connects NP students with vetted inpatient psychiatry preceptors, handles contracts, and ensures clinical hours count—so you can create your free account and secure your placement with confidence.
Why Inpatient Psychiatry Matters in PMHNP Clinical Rotations
The demand for behavioral health services is higher than ever, yet the supply of mental health providers hasn’t kept pace.
Hospitals across the country are grappling with shortages of psychiatrists, while the need for specialized psychiatric care continues to rise. This gap is especially visible in inpatient units, where patients experiencing severe mental disorders, such as bipolar disorder, schizophrenia, major depression, and suicidal ideation require immediate stabilization and continuous oversight.
This is where PMHNP students come in. As part of their nurse practitioner programs, they complete clinical rotations in inpatient psychiatry, gaining the hands-on experience needed to support psychiatrists and the broader care team.
Nurse practitioners bring clinical expertise in psychiatric assessments, medication management, therapy, and patient care, making them essential partners in hospital-based psychiatric services.
Studies show that PMHNPs are already expanding access in rural areas, with their share of mental health prescriber visits increasing from 12.5% to nearly 30% in less than a decade. On the inpatient side, their role is just as critical, allowing hospitals to run efficient, patient-centered psychiatric facilities that meet the growing mental health needs of their communities.
For nurse practitioner students, inpatient rotations are not just a box to check in the placement process. They are where future practitioners learn to work in high-acuity mental health settings, collaborate with psychiatrists, social workers, and other providers, and develop the confidence to handle some of the most challenging psychiatric conditions.
In this blog, we’ll break down what inpatient psychiatry really is, what PMHNP students can expect during their clinical placements, the challenges they may face, and how to secure the right clinical sites and preceptors to guide their journey.
If you’re already beginning your search for inpatient psychiatry rotations, you can create your free NPHub account to explore vetted preceptors and clinical sites that accept students, so you can move forward with confidence.
What Is Inpatient Psychiatry?
Inpatient psychiatry refers to hospital-based care for individuals experiencing acute psychological or emotional distress that cannot be managed in outpatient treatment.
Unlike primary care or outpatient clinics, these are highly structured, congregate environments where patients live together in a unit under 24/7 supervision. The goal is stabilization, whether that means addressing a psychiatric crisis, managing severe psychiatric symptoms, or preventing immediate harm.
Because of the acuity, inpatient psychiatry comes with unique challenges. Safety is a central concern: providers must carefully manage risks like medication errors, seclusion, or re-traumatization during involuntary admissions.
Research also shows patients leaving psychiatric facilities face disproportionately high suicide rates, readmission risks, and gaps in mental health services such as timely 30-day follow-up care. For these reasons, the quality of inpatient psychiatry depends not just on medical interventions but on the environment of care.
That’s where patient-centered care (PCC) becomes crucial. Studies highlight that when psychiatric providers deliver respectful, transparent, and coordinated care that prioritizes patient preferences, outcomes improve dramatically and they are more likely to trust providers, engage in treatment, and continue with follow-up care voluntarily after discharge.
But what exactly does the role of a PMHNP look like inside an inpatient unit, and how do students contribute meaningfully during these rotations? Let’s break it down.
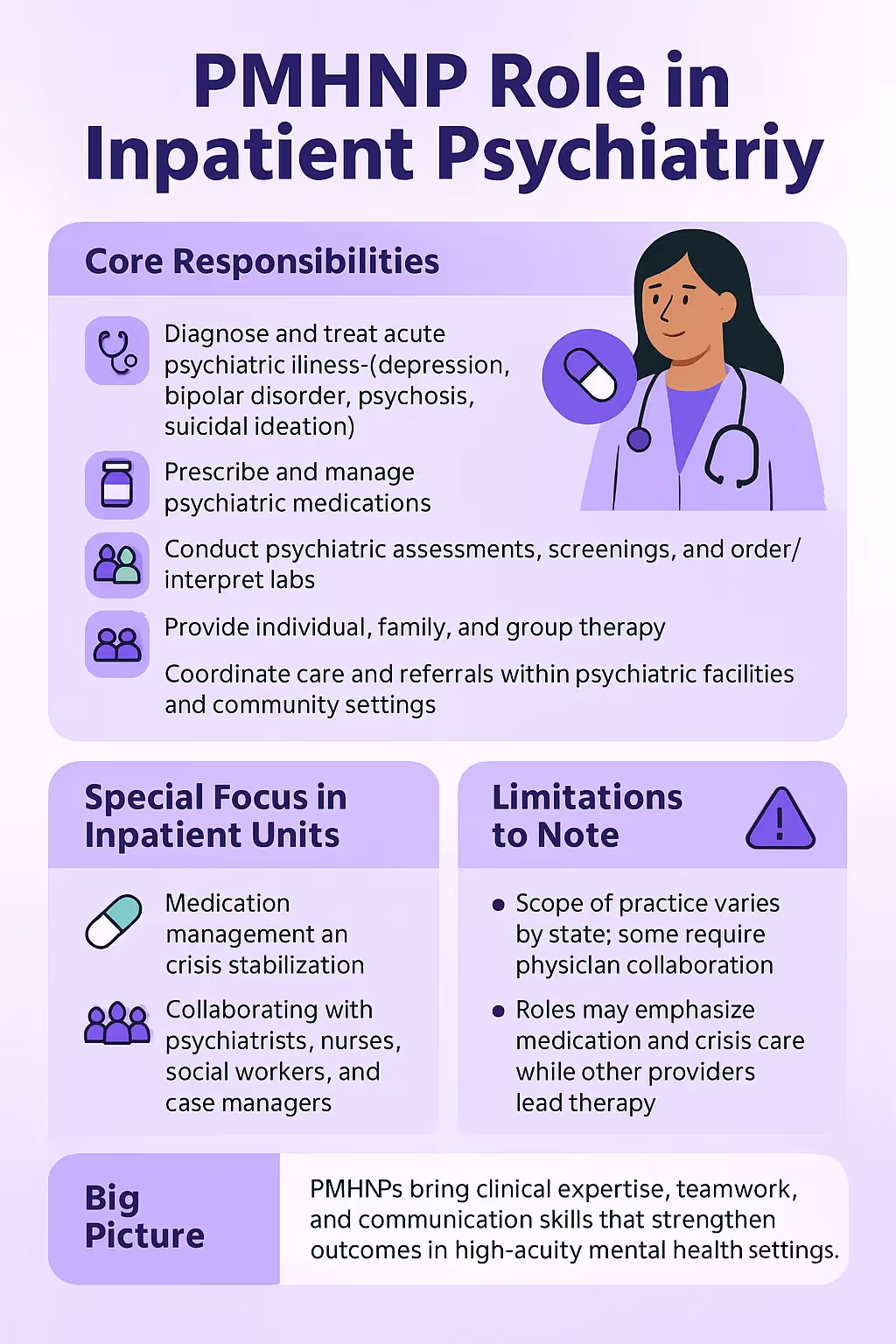
The Role of PMHNPs in Inpatient Psychiatry
In an inpatient unit, the role of a Psychiatric Mental Health Nurse Practitioner (PMHNP) is to provide frontline psychiatric care alongside psychiatrists and the broader treatment team. Their scope is comprehensive and extends well beyond routine patient management.
PMHNPs in inpatient psychiatry are trained to:
- Diagnose and treat acute psychiatric illness such as schizophrenia, bipolar disorder, severe depression, and suicidal ideation.
- Prescribe and manage psychiatric medication to stabilize patients during crisis.
- Provide psychotherapy, including individual, family, and group therapy, in collaboration with other providers.
- Perform psychiatric assessments, screenings, and order/interpret labs to inform treatment.
- Coordinate care and referrals across psychiatric facilities, community-based programs, and follow-up services.
Because therapy is often provided by psychologists or social workers, PMHNPs in inpatient psychiatry frequently take the lead on medication management and crisis stabilization, while maintaining a collaborative role within the team. They also serve as consultants to other departments, such as the emergency room, where quick psychiatric input can be life-saving.
Importantly, scope of practice varies by state. In some regions, PMHNPs can practice independently, while in others, physician collaboration is required. Regardless of the model, their contribution to behavioral health services in inpatient settings has proven essential to meeting patient demand and supporting overextended psychiatrists.
PMHNPs bring clinical expertise, teamwork, and patient-centered communication to the inpatient unit, qualities that not only improve efficiency but also strengthen psychiatric care outcomes for some of the most vulnerable mental health patients.
If you’re preparing to train in this environment, you can create your free account with NPHub to start exploring inpatient psychiatry preceptors and clinical sites that accept students.
What to Expect During Your Inpatient Psychiatry Clinical Rotation
For PMHNP students, inpatient psychiatry clinicals are often the first true immersion into hospital-based mental health care.
Unlike outpatient treatment, where patients are seen for scheduled visits, the inpatient unit runs around the clock. Patients are admitted in crisis, whether due to suicidal ideation, severe bipolar disorder, acute depression, or psychosis, and your role as a student is to learn how these crises are stabilized through structured care.
During your rotation, you can expect to:
- Conduct psychiatric assessments and screenings under supervision.
- Participate in medication management, learning how adjustments are made in acute situations.
- Observe and contribute to treatment team meetings, where psychiatrists, PMHNPs, nurses, and social workers coordinate care.
- Gain exposure to individual and group therapy sessions, even if you are not the primary provider.
- Learn the legal and ethical considerations of involuntary admissions and patient rights.
At the same time, there are real challenges built into these clinical experiences. Training opportunities in inpatient psychiatry are often limited, and nurse practitioner programs vary widely in how much exposure they provide.
Some students may spend more time in outpatient or primary care, leaving gaps in hands-on experience with high-acuity psychiatric patients.Other barriers include:
- Limited clinical placements: Not every school has access to robust inpatient units or specialized pediatric/adolescent programs, making it harder for students to get the full spectrum of inpatient exposure.
- Few fellowship opportunities: Unlike physicians, PMHNPs have very few residency or fellowship programs available in psychiatry, leaving students to rely heavily on clinical rotations for advanced training.
- Balancing academic demands: With many programs shifting from MSN to DNP, students juggle coursework, research projects, and clinical hours. This can reduce the time available to fully engage in inpatient psychiatry clinicals.
- Knowledge gaps: While psychiatric providers in hospitals need advanced skills in psychopharmacology and psychotherapy, not all programs provide standardized training in these areas. This can leave students underprepared for the complexity of managing psychiatric conditions like autism spectrum disorder, eating disorders, or severe mood disorders in the inpatient setting.
In short, an inpatient psychiatry rotation offers some of the most valuable clinical practice a PMHNP student can get but it also exposes the structural gaps in current nurse practitioner education.
That’s why the quality of your clinical site and preceptor matters so much. A strong preceptor won’t just supervise your clinical hours, they’ll actively shape your ability to practice safely, confidently, and compassionately in high-pressure mental health settings.
If you’re looking forward to gain that level of exposure, you can create your free NPHub account and connect with vetted inpatient psychiatry preceptors who provide students with meaningful, structured learning experiences in real hospital settings.
Securing PMHNP Clinical Rotations in Inpatient Psychiatry
Securing an inpatient psychiatry preceptor isn’t like finding a placement in a primary care clinic. These rotations happen in high-security environments where patient safety is paramount, and that means tighter rules, fewer open slots, and a more complicated approval process.
Many psychiatric facilities require credentialing, orientation, and formal contracts before a student can even step onto the unit. For PMHNP students, the search can feel like a locked door, you know the training is critical, but getting access is the real challenge.
That doesn’t mean it’s impossible. Students who approach the search with strategy and persistence often break through the barriers. Here are five inpatient-specific approaches that can make the difference:
1. Learn how hospitals handle student onboarding.
Unlike community clinics, inpatient units usually require background checks, credentialing, and orientation before you can step foot on the floor. Contact the hospital’s medical education office or nursing education department to ask about their student onboarding process before approaching potential preceptors. This shows you understand the system and saves time chasing dead ends.
2. Approach psychiatrists through professional associations.
Hospital psychiatrists and PMHNPs often belong to local or state chapters of groups like the American Psychiatric Association or nurse practitioner organizations. Attending a meeting, webinar, or networking event can help you connect with providers who are open to precepting but don’t advertise it.
3. Look at teaching hospitals and residency programs.
Facilities that train psychiatry residents or psychology interns are often more open to taking NP students. They already have the infrastructure for supervision, documentation, and student learning. Even if your preceptor isn’t a psychiatrist, you may find nurse practitioners on staff who regularly teach.
4. Frame your ask around value, not need.
When you reach out, don’t just say, “I need a preceptor.” Emphasize how students contribute: helping with psychiatric assessments, supporting documentation, or lightening the load during busy inpatient shifts. Positioning yourself as an asset increases your chances of being accepted.
5. Research smaller or specialized inpatient units.
Large psychiatric hospitals are often saturated with student requests. Smaller units—such as geriatric, adolescent, or dual-diagnosis inpatient units—may have fewer applicants and more room for motivated students. Be specific in your outreach: “I’m interested in rotations that focus on crisis stabilization and psychiatric medication management.”
Red Flags in the Inpatient Psychiatry Preceptor Search
Not every opportunity in inpatient psychiatry will set you up for success. Because these rotations require structured, hospital-based clinical experiences, the wrong site or preceptor can leave you with wasted hours—or worse, no approval from your school. Here are the key red flags to watch for:
1. Preceptors without inpatient authority.
A common pitfall for students is finding a preceptor who is technically licensed but doesn’t have the authority to involve you in true inpatient psychiatry. If they lack admitting privileges, access to hospital units, or oversight within a psychiatric facility, your role may be reduced to observing conversations or paperwork instead of direct patient care. This severely limits your exposure to the real challenges of an inpatient unit.
Even worse, these limitations can result in your hours being rejected by your school. If your clinical site doesn’t meet accreditation or program standards, all the time you spend there could be wasted. Always confirm up front that your preceptor has the proper credentials and hospital access to provide a legitimate, approved clinical experience.
2. Sites with little or no exposure to acute psychiatric care.
Not every psychiatric site qualifies as a true inpatient environment. Some facilities may operate more like residential programs or group therapy centers, where you won’t see acute cases such as suicidal ideation, severe bipolar disorder, or psychosis. While those settings may still provide value, they often don’t meet the criteria for an inpatient psychiatry rotation.
To avoid this, make sure your rotation will include hands-on experiences with psychiatric assessments, medication management, and crisis stabilization. If a site tells you your role will be limited to observing therapy groups or reviewing charts, that’s a red flag that it won’t give you the exposure your PMHNP program requires.
3. Facilities unwilling to formalize the placement.
Hospitals operate under strict compliance standards, and every valid student placement requires contracts, site agreements, and liability paperwork between your school and the facility. If a site seems hesitant or unwilling to move forward with this step, it signals potential problems ahead.
Even if a provider seems enthusiastic about teaching, without signed agreements your school will almost certainly reject the placement. Students often waste weeks of effort in these situations, only to learn the facility can’t or won’t finalize the paperwork. Always ask early in the process if the site is willing to engage in the formal placement process.
4. Unstructured or “shadow-only” supervision.
Some preceptors may allow you on the unit but keep your role passive. If you’re only watching from the sidelines, without opportunities to practice psychiatric assessments, write notes, or engage with patients, your clinical skills won’t grow. Shadowing has its place, but a full rotation requires active learning under supervision.
This lack of structure often reflects poor preceptor planning. A strong preceptor should be able to outline what your responsibilities will look like week to week. If they can’t tell you how you’ll gain exposure to psychiatric care tasks—beyond simply observing—consider it a warning sign that your experience will fall short.
5. Overpromising without clarity.
Some preceptors may sound enthusiastic at first but fail to provide concrete details about your role. You may hear promises like, “We’ll figure it out once you start,” or vague assurances about learning opportunities without specifics. In the high-pressure environment of an inpatient unit, lack of clarity usually translates into missed opportunities.
Instead, look for a preceptor who can clearly explain what your learning experience will include: crisis stabilization, medication management, team meetings, and discharge planning. If they can’t provide that level of detail before you begin, there’s a good chance the rotation won’t give you the structured exposure you need.
Spotting these red flags early can save you from wasted hours, denied placements, and overwhelming stress. But for many PMHNP students, knowing what to look for isn’t the hardest part, finding a qualified inpatient psychiatry preceptor is the real challenge. That’s where professional support can make all the difference.
How To Secure Clinical Rotations as An Inpatient Psychiatry Nurse Practitioner?
If the DIY search for an inpatient psychiatry preceptor feels like a maze, that’s because it is. Between limited clinical sites, paperwork hurdles, and uncertainty about whether your hours will count, many PMHNP students end up frustrated and behind schedule.
That’s why more students are turning to professional preceptor matching services, because the right support can take the stress out of the placement process and keep your education on track.
At NPHub, we simplify the search by connecting nurse practitioner students with vetted psychiatric providers in real inpatient units. Instead of chasing unresponsive leads or worrying about red flags, you gain access to a trusted network of preceptors who are ready to teach.
Every provider in our network has been reviewed for experience, licensure, and ability to supervise clinical rotations that meet school and accreditation standards. We handle contracts, liability forms, and agreements with your school so you don’t risk having hours rejected.
Unlike shadow-only placements, our clinical placements ensure students gain exposure to psychiatric assessments, medication management, crisis stabilization, and patient care. Instead of spending months on unanswered emails, you can secure a psychiatric facility placement faster and with confidence.
You’ll know your clinical hours are counting toward your PMHNP program requirements and preparing you for national certification.
The reality is simple: without the right preceptor, your clinical experiences can feel unstructured, stressful, or even wasted. With NPHub, you don’t just get a placement, you get a guided path into the kind of clinical practice that builds your skills and prepares you to serve patients in high-acuity mental health settings.
If you’re ready to move forward, you can create your free NPHub account today and start exploring vetted inpatient psychiatry preceptors in hospitals and behavioral health facilities near you.
Preparing for Success in Your PMHNP Clinicals
Completing your PMHNP clinicals in an inpatient psychiatry setting is a defining moment in your journey as a future mental health provider.
These rotations put you face-to-face with patients in their most vulnerable moments: the individual experiencing suicidal ideation, the young adult in the grips of bipolar disorder, the older patient struggling with treatment-resistant depression. Here, the theories you’ve studied in your nurse practitioner program finally meet the unpredictable reality of human suffering, crisis, and recovery.
And yet, this is also where the challenges are greatest. Unlike outpatient treatment, inpatient psychiatry demands that you learn how to think and act quickly under pressure, collaborate across multidisciplinary teams, and balance compassion with clear clinical decision-making.
These are not skills you can pick up from textbooks or lectures—they are forged in the hospital hallways, team meetings, and patient encounters of your clinical rotations. But while the importance of inpatient psychiatry is clear, the placement process often feels anything but.
Students chase leads that go nowhere, spend hours cold-calling hospitals that don’t even accept students, or discover too late that their site doesn’t qualify for program credit. These barriers don’t just cost you time; they put your graduation date, licensure, and future patient care at risk.
That’s why the preceptor you secure matters so much. The right inpatient psychiatry preceptor will not only guide you through medication management, crisis stabilization, and psychiatric assessments, they’ll help you see what excellent psychiatric care looks like when the stakes are highest. They’ll show you how to earn trust from patients who feel powerless, how to navigate the tension between safety and autonomy, and how to practice with empathy without burning out.
The truth is, no PMHNP should have to gamble their education on an uncertain search. With the demand for behavioral health services rising nationwide and psychiatrists stretched thin, the healthcare system needs the next generation of psychiatric providers prepared and confident. And that means ensuring students have access to meaningful, structured clinical experiences in inpatient psychiatry.
At NPHub, that’s exactly what we do. By connecting students with vetted psychiatric providers in approved clinical settings, handling the paperwork, and securing placements that count toward your clinical hours, we take the uncertainty out of the process. What you’re left with is the chance to focus fully on your learning experience, to step into your inpatient rotation ready to grow, serve, and succeed.
And if you want proof that this works, you don’t have to take our word for it. You can explore our reviews and hear directly from NP students who were once in your shoes, struggling to find placements, and now sharing how NPHub helped them secure the rotations they needed. Their stories show what’s possible when you stop searching alone and start working with a team that understands the process.
Plus, every student is protected by our Perfect Preceptor Promise: if a preceptor ever falls through, we’ll find you a replacement at no extra cost. That means your investment, and your graduation timeline, are always safe.
If you’re serious about preparing for your future as a psychiatric mental health nurse practitioner, now is the time to take control of your placement journey. Create your free NPHub account and move one step closer to the inpatient psychiatry rotation that will shape not just your education, but your career.
Frequently Asked Questions: PMHNP Clinicals in Inpatient Psychiatry: What to Expect
1. Do inpatient psychiatry rotations count toward my PMHNP clinical hours?
Yes. Inpatient psychiatry clinicals are widely accepted by nurse practitioner programs as part of the required clinical hours. They provide essential training in acute care, crisis management, and psychiatric assessments—skills that are vital for your national certification. Always confirm with your school’s clinical coordinators to ensure the site meets program requirements.
2. What types of patients will I encounter in an inpatient psychiatry rotation?
You’ll work with psychiatric patients experiencing acute crises, including suicidal ideation, bipolar disorder, severe depression, psychosis, substance use, and anxiety disorders. Some inpatient units specialize in populations like adolescents, older adults, or dual-diagnosis patients, offering exposure to diverse psychiatric conditions.
3. How are inpatient psychiatry rotations different from outpatient treatment?
In outpatient care, patients are seen on a scheduled basis, often for ongoing medication management or therapy. In inpatient psychiatry, patients are hospitalized for crisis stabilization, meaning the pace is faster, the cases more severe, and collaboration with a multidisciplinary team (psychiatrists, nurses, social workers) is constant.
4. Will I get hands-on experience or mostly shadow in inpatient psychiatry?
A high-quality inpatient rotation should include direct involvement in psychiatric assessments, treatment planning, documentation, and medication adjustments under supervision. If your role is limited to shadowing, it may not provide the clinical expertise needed for your PMHNP program.
5. What skills should I expect to develop during my inpatient psychiatry clinicals?
Key skills include crisis intervention, psychiatric evaluation, medication management, documentation in hospital records, and interdisciplinary collaboration. You’ll also gain experience in balancing patient safety with autonomy, an essential skill in behavioral health services.
6. Are all nurse practitioner students required to do inpatient psychiatry rotations?
Some PMHNP programs mandate inpatient experience, while others allow substitutions with outpatient or community psychiatry. However, most clinical coordinators strongly recommend inpatient exposure, since it prepares students for the full spectrum of mental health care.
7. What challenges do NP students face in inpatient psychiatry?
Common challenges include navigating involuntary admissions, handling emotionally intense cases, and managing limited time with patients. Logistically, securing a clinical placement in a hospital setting can be difficult due to strict credentialing and limited clinical sites.
8. Can I do my inpatient rotation in any psychiatric facility?
Not every psychiatric facility qualifies. To meet program standards, the site must provide structured supervision, opportunities for direct patient care, and exposure to acute psychiatric conditions. Be cautious of facilities that lack a clear training plan or won’t complete school-required paperwork.
9. How do I prepare before starting an inpatient psychiatry rotation?
Review your knowledge of common psychiatric disorders, especially depression, bipolar disorder, schizophrenia, and substance use disorders. Refresh your understanding of psychotropic medications and crisis protocols. It also helps to build confidence in documentation and communication with interdisciplinary teams.
10. How can NPHub help me secure an inpatient psychiatry preceptor?
With NPHub, you don’t have to navigate the search alone. We connect you with vetted psychiatric providers in inpatient units, handle contracts and agreements with your school, and ensure the rotation counts toward your required hours. You can create your free NPHub account today to explore available clinical sites and lock in a placement that prepares you for certification and practice.
Key Definitions: Inpatient Psychiatry Clinicals for PMHNP Students
- Inpatient Psychiatry
Hospital-based psychiatric care where patients experiencing acute mental illness or crises are admitted for stabilization, monitoring, and treatment. - Inpatient Unit
A structured, hospital-based environment where psychiatric patients live together under 24/7 care. Units may specialize in adult, adolescent, or geriatric populations. - Crisis Stabilization
The immediate interventions used in inpatient psychiatry to reduce the risk of harm in patients experiencing severe psychiatric symptoms, such as suicidal ideation or psychosis. - Psychiatric Assessment
A comprehensive evaluation conducted by providers—including PMHNPs—that collects information on symptoms, history, and functioning to guide treatment planning. - Medication Management
The prescribing, monitoring, and adjusting of psychiatric medication to stabilize acute conditions. A core responsibility of PMHNPs in inpatient psychiatry. - Interdisciplinary Team
The group of professionals—psychiatrists, PMHNPs, nurses, social workers, case managers, and therapists—who collaborate on patient care in inpatient psychiatry. - Involuntary Admission
A legal process in which a patient is admitted to a psychiatric facility against their will due to risk of harm to themselves or others. PMHNP students often learn how to navigate the ethical and clinical challenges of these cases. - Discharge Planning
The process of preparing patients to leave an inpatient unit, which includes care coordination, referrals to outpatient treatment, and ensuring continuity of care. - Clinical Placement
A supervised rotation in a healthcare setting that allows NP students to apply their classroom knowledge in real-world psychiatric care under the guidance of a preceptor. - National Certification (PMHNP-BC)
The certification exam for Psychiatric-Mental Health Nurse Practitioners. Clinical hours completed in settings like inpatient psychiatry are required to sit for the exam and practice as a certified provider.
About the author
- NPHub Staff
At NPHub, we live and breathe clinical placements. Our team is made up of nurse practitioners, clinical coordinators, placement advisors, and former students who’ve been through the process themselves. We work directly with NP students across the country to help them secure high-quality preceptorships and graduate on time with confidence. - Last updated
October 3, 2025 - Fact-checked by
NPHub Clinical Placement Experts & Student Support Team - Sources and references
- https://www.signethealth.com/2024/05/22/incorporating-psychiatric-nurse-practitioners-on-inpatient-units-is-a-game-changer/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10986256/pdf/qxad017.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7547148/pdf/nihms-1616484.pdf
- https://www.nphub.com/perfect-preceptor-promise
Find a preceptor who cares with NPHub
Book a rotation.webp)








.webp)


.webp)


%20(3)%20(2).svg)
.webp)