TL;DR – Benefits of Full Practice Authority for Nurse Practitioners: 5 Key Reasons
- NPs close the healthcare access gap. With physician shortages rising, especially in rural areas, Full Practice Authority (FPA) allows NPs to step in and provide timely, essential primary care—no physician sign-off required.
- It lowers costs while keeping care quality high. FPA removes unnecessary oversight, reducing administrative burdens and healthcare costs—without compromising outcomes.
- NPs deliver patient-centered care that improves outcomes. Studies show NP care equals or exceeds physician care in quality, with stronger focus on prevention and health education.
- FPA boosts patient satisfaction. Patients treated by NPs report shorter wait times, longer visits, clearer communication, and higher satisfaction overall, especially in underserved regions.
- It opens doors for NP leadership and growth. FPA lets NPs run independent practices, lead teams, and drive innovation in care delivery—maximising their impact across the system.
Take a break from your arduous studies and imagine the moment when you confidently step into the world of healthcare, wearing your white coat and stethoscope. As you consider the vivid imagery, think about the many paths your career as a Nurse Practitioner (NP) could take.
Full Practice Authority (FPA) isn’t just industry jargon—it’s a game-changer in primary care and health care delivery. As an aspiring NP, embracing FPA could be more than just a possibility; it could be your key to making a significant impact. However, it's important to understand that some states have restricted practice authority, which imposes limitations on NPs compared to those with full practice authority.
In today’s healthcare landscape, marked by increasing demands, rising costs, and a growing emphasis on quality care, the concept of nurse practitioners practicing independently has gained considerable attention. The push for expanded nurse practitioner roles and relaxing occupational licensing requirements is reshaping our approach to healthcare.
As advocates for Full Practice Authority at NPHub, we believe it’s crucial to explore the compelling reasons why nurse practitioners should have the opportunity to practice independently. Let’s dive into the benefits of full practice authority for nurse practitioners and how it can transform health care services, particularly in rural and underserved areas.
Introduction: Understanding Full Practice Authority
Full practice authority (FPA) is a crucial aspect of healthcare delivery, enabling advanced practice registered nurses (APRNs), including nurse practitioners (NPs), to provide high-quality healthcare services to patients. FPA allows NPs to practice independently, making decisions and taking actions without the need for physician supervision. This authority is essential for improving health outcomes, particularly in rural and underserved areas where access to healthcare is limited.
Imagine being able to make clinical decisions, prescribe medications, and manage patient care autonomously. This is the reality for nurse practitioners with full practice authority. By eliminating the need for physician oversight, FPA empowers NPs to utilize their extensive training and expertise to the fullest extent, ensuring that patients receive timely and effective care. This is especially vital in rural and underserved areas, where healthcare providers are often scarce, and the demand for primary care services is high.
What is Full Practice Authority?
Full practice authority is the authorization of NPs to evaluate patients, diagnose, order and interpret diagnostic tests, and initiate and manage treatments, including prescribing medications. This authority is granted by the state board of nursing and is considered the exclusive licensure authority for NPs. FPA enables NPs to practice independently, providing primary care services to patients without the need for physician supervision.
Think of it as a green light for nurse practitioners to fully engage in patient care without the red tape of physician supervision. This autonomy not only streamlines healthcare delivery but also enhances the efficiency and responsiveness of the healthcare system. By allowing NPs to practice independently, states with full practice authority can better meet the healthcare needs of their populations, particularly in areas where access to physicians is limited.
Definition and Scope
Full practice authority is defined as the ability of NPs to provide healthcare services to the full extent of their education, training, and licensure. This includes the authority to:
- Evaluate patients and diagnose medical conditions
- Order and interpret diagnostic tests
- Initiate and manage treatments, including prescribing medications
- Provide primary care services to patients
The scope of FPA varies by state, with some states granting full practice authority to NPs and others imposing restrictions on their practice. However, research has shown that states with full practice authority for NPs have better health outcomes, lower healthcare costs, and improved access to primary care services.
In states where NPs have full practice authority, patients benefit from more accessible and cost-effective care. These states often see lower healthcare costs and improved health outcomes, as NPs can provide comprehensive care without the delays and additional costs associated with physician supervision. By embracing full practice authority, we can create a more efficient and effective healthcare system that meets the needs of all patients, regardless of their location.
2025 Progress on Full Practice Authority: Historic Milestone for Nurse Practitioners
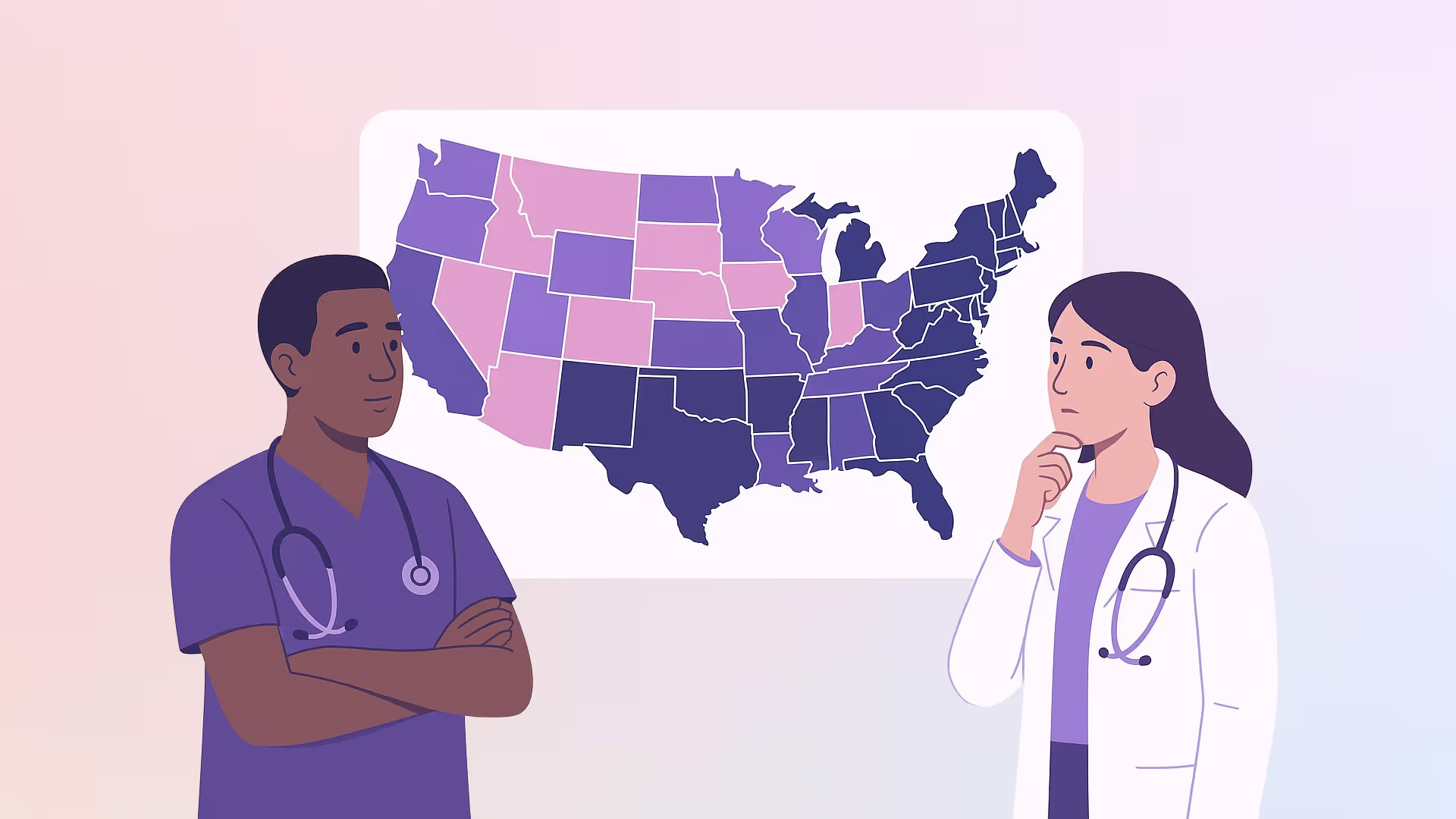
The landscape of nursing practice and healthcare delivery in the United States has changed dramatically in recent years. As of 2025, 34 states plus Washington, D.C., now recognize Full Practice Authority (FPA) for nurse practitioners (NPs) — a pivotal milestone that’s reshaping the future of primary care providers across America.
This expansion of practice authority is more than just a legislative win; it's a victory for patient care, healthcare access, and the ability to improve health outcomes, especially in rural and underserved areas.
What Full Practice Authority Means for Advanced Practice Registered Nurses (APRNs)
Full Practice Authority empowers advanced practice registered nurses, including nurse practitioners, certified nurse midwives, and clinical nurse specialists, to:
- Evaluate patients independently
- Order and interpret diagnostic tests without unnecessary physician sign-offs
- Prescribe medications, including Schedule II controlled substances, where permitted
- Initiate and manage treatment plans without physician supervision
- Fully operate under the exclusive licensure authority of the state board of nursing, not under collaborative agreements with physicians
Essentially, Full Practice Authority allows NPs to practice independently, applying the full scope of their education and training without outdated bureaucratic restrictions.
By eliminating restricted practice authority and reducing collaborative practice agreements, more states are tapping into the full potential of nurse practitioners to deliver timely, affordable, and high-quality health care services across rural and urban communities.
Newly Transitioned Full Practice Authority States (2020–2025)
Between 2020 and 2025, the following states granted Full Practice Authority to NPs:
- Massachusetts
- Pennsylvania
- Kansas
- Ohio
- Texas
- Indiana
- Tennessee
- Michigan
- Alabama
- Louisiana
- South Carolina
- Wisconsin
This wave of reform strengthens the argument that relaxing occupational licensing requirements is not about diminishing patient safety — it's about expanding health resources and empowering highly trained NPs to treat patients effectively, particularly in rural areas.
Why Full Practice Authority Matters Now More Than Ever
1. Solving the Healthcare Access Crisis
With a rapidly aging population, widespread health professional shortages, and the rising costs of health care utilization, primary care nurse practitioners are essential in filling gaps left by primary care physicians.
FPA allows NPs to deliver primary care services directly to Medicaid patients, Medicare beneficiaries, and veterans without the delays caused by physician oversight.
2. Enhancing Health Outcomes in Underserved Areas
Rural and underserved areas tend to face some of the most severe health disparities.
In states with full practice authority, rural residents report higher access to preventive care, better management of chronic diseases like hypertension and diabetes, and higher patient satisfaction.
Nurse practitioners in rural areas have become a cornerstone of rural health, offering a lifeline where physician assistants and doctors are scarce.
3. Strengthening the Healthcare Workforce
Granting full practice authority for nurse practitioners makes the healthcare system more flexible and resilient.
It allows nurse practitioners, NPs, and physician assistants, and other advanced practice providers to innovate in telehealth, chronic disease management, and mental health services — all without unnecessary bottlenecks in patient care.
4. Improving Economic Efficiency
One of the major benefits of full practice authority for nurse practitioners is its positive impact on health economics.
By eliminating duplicative oversight requirements, states lower administrative costs and streamline healthcare services, leading to:
- Fewer delays in patient care
- Lower overall costs for health services administration
- Expanded care for Medicare beneficiaries and Medicaid patients
And importantly: no compromise on patient outcomes.
Even with this incredible progress, 12 states still operate under reduced practice authority, and 4 states maintain restricted practice authority.
However, experts in nursing regulation predict that national FPA standardization could happen within the next 5–7 years.
Emerging trends include:
- Federal standardization efforts for NPs working with veterans affairs patients and telehealth expansion
- Policy initiatives supporting pay parity for NPs and physicians delivering equivalent primary healthcare
- Increased focus on expanding the physician assistant scope of independent practice, mirroring NP advancements
Reason 1: Addressing the Healthcare Shortage through Full Practice Authority
If you’ve ever found yourself in a seemingly endless queue at a healthcare facility, you’ve experienced firsthand the impact of our nation’s healthcare shortage. This growing crisis underscores the benefits of full practice authority for nurse practitioners.
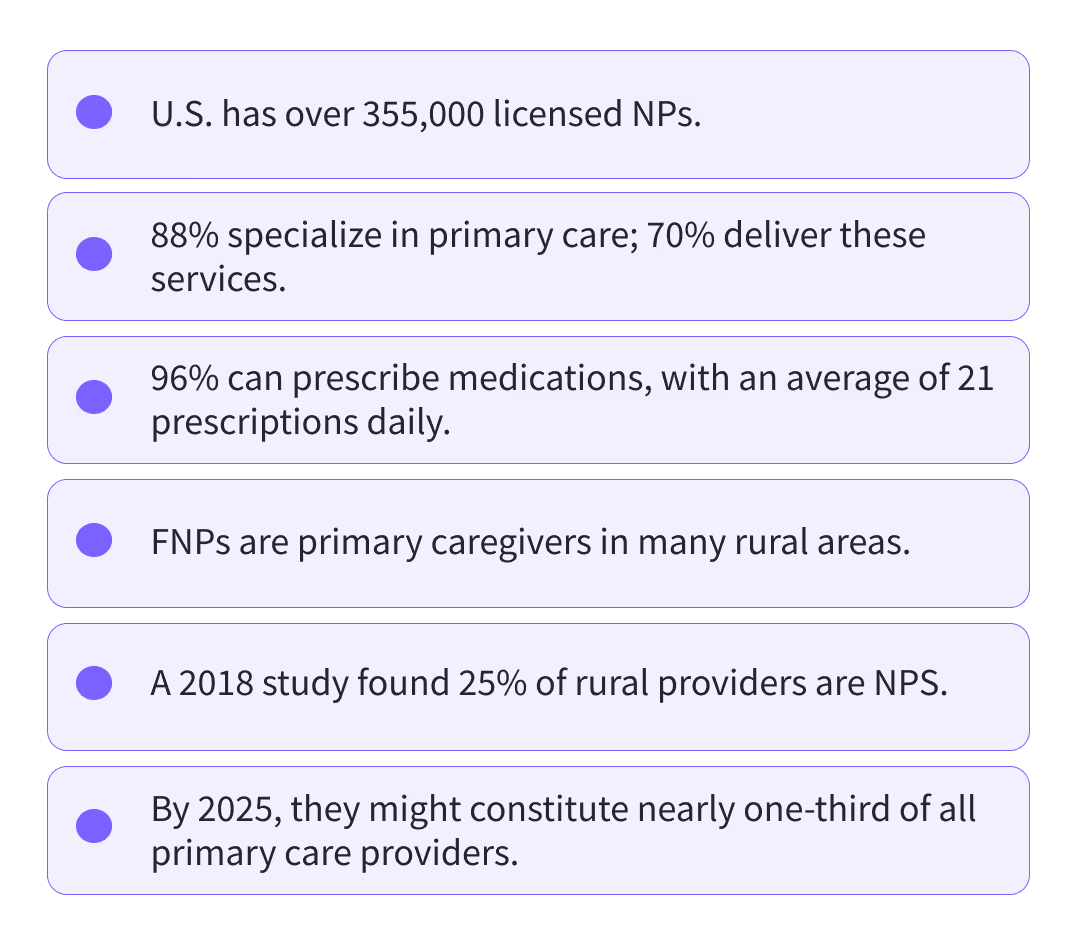
With our aging population and the increasing prevalence of chronic diseases, the demand for healthcare services is skyrocketing. Here’s a quick overview of the situation:
Shortage Reality: According to the American Medical Colleges, by 2034, the U.S. could face a deficit of up to 48,000 primary care physicians.
Worst Affected: In 2021, nearly 95 million Americans lived in health professional shortage areas, with 65% residing in rural regions where access to health care providers is particularly limited.
Why the Shortage?
- Growing medical sub-specialties draw physicians away from primary care.
- The aging U.S. population requires more healthcare services.
- Many primary care physicians are nearing retirement.
A wealth of studies confirm that nurse practitioners offer cost-efficient and consistently high-quality patient care. This is why granting NPs full practice authority emerges as a critical solution to these challenges:
- NPs can help improve health outcomes in underserved areas.
- They can reduce healthcare costs while maintaining quality of care.
- NPs excel in providing primary care services, helping to fill the gap left by the physician shortage.
In conclusion, nurse practitioners practicing independently are indispensable in bridging these healthcare gaps. Their comprehensive skill set and emphasis on preventive care position them as pivotal figures in the evolving healthcare landscape. By allowing NPs to practice to the full extent of their education and training, we can significantly enhance health care access and improve patient outcomes, particularly in rural areas and for underserved populations.
Reason 2: Cost-Effective Healthcare Through Nurse Practitioner Independence
In the realm of healthcare, cost and quality are two critical factors. The soaring costs of health care services have become a significant concern for patients, providers, and policymakers alike. Wouldn't it be fantastic if there was a solution that could provide high-quality care without breaking the bank? Well, guess what? The benefits of full practice authority for nurse practitioners might just be the answer we've been seeking.
Several studies have shown that nurse practitioners' care is not only comparable in quality to that of physicians but also more cost-effective. Yes, you read that right! NPs offer a more economical solution without compromising on the quality of patient care.
They achieve this cost-effectiveness in various ways:
- Focusing on preventive care and health promotion, which can reduce hospitalizations and emergency room visits.
- Efficient utilization of health resources, including appropriate ordering of diagnostic tests and prescribing medications.
- Streamlined processes thanks to full practice authority, which eliminates the need for physician oversight and collaborative practice agreements in many cases.
By reducing the financial burden on patients and healthcare systems, nurse practitioners practicing independently drive a much-needed change in our healthcare landscape. They're helping to make healthcare more accessible and affordable, particularly in rural and underserved areas, ensuring that no one is left behind in receiving the care they need and deserve.
The impact of NPs on healthcare costs is particularly noteworthy:
- NPs often spend more time with patients, potentially leading to better health outcomes and reduced long-term costs.
- In states with full practice authority, there's evidence of improved healthcare access without increased costs.
Isn't this cost-effective approach, combined with high-quality care, the essence of truly exceptional healthcare? As we continue to grapple with rising healthcare costs, the expanded role of nurse practitioners through full practice authority presents a promising solution that benefits both patients and the healthcare system.
Reason 3: High-Quality Patient Care Through Full Practice Authority
It's time for a moment of truth — the quality of patient care is the backbone of a thriving healthcare system. Without it, all other efforts pale into insignificance. When we discuss the benefits of full practice authority for nurse practitioners, high-quality patient care is at the forefront of the conversation.
Nurse practitioners, with their rigorous education and clinical training, are well-equipped to deliver top-notch patient care. They bring a unique blend of medical competence and a holistic, patient-centered approach that sets them apart in healthcare.
Studies have consistently shown that NPs provide care that is comparable to, and in some cases superior to, that of physicians. This is particularly true in primary care settings, where nurse practitioners excel in:
- Evaluating patients comprehensively
- Interpreting diagnostic tests accurately
- Prescribing medications appropriately
- Providing thorough patient education
Additionally, NPs have a particular knack for preventive care and health promotion — two pillars of high-quality healthcare. They emphasize not just treating diseases but preventing them from occurring in the first place. This preventive approach contributes to better health outcomes and a healthier population, especially in rural and underserved areas where access to healthcare can be limited.
It's safe to say that nurse practitioners with full practice authority aren't just treating symptoms — they're transforming lives. By allowing NPs to practice to the full extent of their education and training, we're not only addressing the primary care shortage but also enhancing the quality of care delivered across the healthcare system.
Reason 4: Enhanced Patient Satisfaction through Nurse Practitioner Independence

Everyone appreciates recognition for a job well done. For nurse practitioners (NPs), that recognition often comes in the form of high patient satisfaction scores, which is another compelling benefit of full practice authority for nurse practitioners.
Numerous studies indicate that NPs consistently receive positive feedback from their patients regarding the quality of care they provide. This satisfaction isn't just a feel-good metric—it's a crucial indicator of healthcare quality and effectiveness.
The success of NPs in achieving high patient satisfaction hinges on several factors:
- Patient-Centered Approach: NPs are trained to provide holistic, patient-centered care that addresses not just physical symptoms but also mental health and social determinants of health.
- Empathetic Care: The nursing background of NPs often translates into a more empathetic and compassionate approach, fostering strong patient-provider relationships.
- Comprehensive Care: As primary care providers, NPs can evaluate patients, interpret diagnostic tests, and prescribe medications, offering comprehensive care under one roof.
- Health Education: NPs excel in patient education, empowering individuals to take an active role in their health management.
Let's not forget the convenience factor. With full practice authority, nurse practitioners can deliver swift, responsive care, ensuring that patients' needs are met promptly. This is particularly crucial in rural and underserved areas where access to healthcare can be limited.
In states with full practice authority, patients often report:
- Shorter wait times for appointments
- Longer consultation times with their healthcare provider
- Clearer explanation of health conditions and treatment plans
- Higher overall satisfaction with their healthcare experience
It's akin to having a personal healthcare companion at your service, adding a cherry to the patient satisfaction sundae. This satisfaction is linked to better health outcomes, improved medication adherence, and more effective management of chronic conditions.
Reason 5: Expanded Professional Growth Opportunities through FPA
If you're a nurse practitioner (NP) or aspiring to become one, you're likely eager to utilize your skills and knowledge to their fullest potential. One of the key benefits of full practice authority for nurse practitioners is that it allows you to do just that and paves the way for professional growth opportunities.
Full practice authority grants NPs the autonomy to:
- Manage their own practice
- Make independent clinical decisions
- Lead healthcare teams
- Evaluate patients comprehensively
- Prescribe medications without physician oversight
- Interpret diagnostic tests independently
This level of independence fosters a sense of professional achievement and significantly contributes to job satisfaction. After all, who doesn't relish the freedom to practice their craft as they deem fit?
The ability to practice independently also opens up new avenues for NPs to specialize and innovate within the healthcare system. From opening their own primary care clinics to pioneering healthcare programs in underserved areas, the sky's the limit for nurse practitioners with full practice authority.
Moreover, full practice authority enables NPs to fully embrace their role as primary care providers, working alongside physicians and other healthcare professionals as equals. This collaborative environment enhances the overall quality of patient care and promotes professional growth through shared knowledge and expertise.
Full practice authority transforms NPs into healthcare trailblazers, leading to a more effective, inclusive, and patient-centered healthcare system. As the healthcare landscape continues to evolve, the expanded role of nurse practitioners through full practice authority presents exciting opportunities for professional development and innovation in patient care delivery.
Navigating Opposition and Challenges to Full Practice Authority
Like any significant change in healthcare policy, expanding full practice authority for nurse practitioners isn't without its challenges. The road to independent practice for NPs is often met with opposition, primarily from physician organizations and medical associations.
Key concerns raised by opponents include:
- Patient safety: Some argue that the difference in training between NPs and physicians could potentially impact patient outcomes.
- Quality of care: Questions arise about whether NPs can provide the same level of comprehensive care as primary care physicians.
- Scope of practice: Debates continue over the appropriate boundaries of NP practice authority.
The American Medical Association, for instance, has expressed reservations about relaxing occupational licensing requirements for NPs, citing concerns about patient safety and the quality of healthcare delivery.
However, the opposition's narrative often overlooks crucial evidence:
- Numerous studies attest to the efficacy and safety of NP care.
- Research consistently shows that NPs provide high-quality primary care, often with patient outcomes comparable to those of physicians.
- In states with full practice authority, there's no evidence of decreased patient safety or compromised care quality.
Real-world practices in states with full practice authority for nurse practitioners demonstrate the value NPs bring to the healthcare system:
- Improved healthcare access, especially in rural and underserved areas
- Cost-effective care delivery without sacrificing quality
- High levels of patient satisfaction
It's essential to view these challenges not as roadblocks but as opportunities for dialogue and education. By presenting evidence-based research and demonstrating the benefits of full practice authority, NPs can effectively counter opposition and pave the way for expanded practice rights.
Strategies to address these challenges include:
- Continuing to conduct and publish high-quality research on NP outcomes
- Engaging in collaborative discussions with physician groups to find common ground
- Educating policymakers and the public about the extensive training and capabilities of NPs
- Highlighting success stories from states with full practice authority
As we move forward, it's crucial to remember that the ultimate goal is to improve health outcomes and increase access to quality care for all patients. By focusing on this shared objective, nurse practitioners can work towards overcoming opposition and achieving full practice authority across all states, ultimately contributing to a more robust and responsive healthcare system.
Moving Forward: Embracing the Benefits of Full Practice Authority for Nurse Practitioners
The path to full practice authority may be challenging, but the view from the top is undoubtedly worth it. It's time for nurse practitioners to buckle up and take the driver's seat in advocating for expanded practice rights. And here's the good news: you're not alone on this journey.
Advocacy and education among advanced practice registered nurses can make a significant difference. By raising awareness about the benefits of full practice authority for nurse practitioners and standing together, NPs can contribute to transforming healthcare delivery.
As we conclude our exploration of why nurse practitioners should practice independently, let's recap the key benefits:
- Addressing healthcare shortages, especially in rural and underserved areas
- Delivering high-quality, cost-effective care
- Improving patient satisfaction and health outcomes
- Fostering professional growth and innovation in healthcare
- Enhancing the overall efficiency of our healthcare system
NPHub stands in solidarity with nurse practitioners advocating for full practice authority. We believe in your potential and the immense value you bring to healthcare. Your unique blend of medical knowledge and patient-centered care makes you invaluable assets in our evolving healthcare landscape.
As we progress, remember that every stride toward full practice authority is a step toward a healthier future for all. Whether it's through state board advocacy, engaging with policymakers, or educating the public, your efforts contribute to a more accessible, efficient, and effective healthcare system.
So, to all nurse practitioners out there: continue to advocate, educate, and demonstrate the high-quality care you provide. Your role in shaping the future of healthcare is crucial, and with full practice authority, your impact can be even greater. Together, we can build a healthcare system that truly puts patients first and maximizes the skills of all healthcare providers.
Frequently Asked Questions (FAQs)
What is Full Practice Authority for nurse practitioners?
Full Practice Authority allows nurse practitioners to practice independently without physician oversight. NPs can evaluate patients, diagnose, prescribe medications, and manage treatment plans under the authority of the state board of nursing.
How many states have Full Practice Authority in 2025?
As of 2025, 34 states plus Washington, D.C. grant Full Practice Authority to nurse practitioners. This number continues to grow as healthcare needs increase.
Does Full Practice Authority compromise patient safety?
No. Multiple studies show that NP-provided care is equal to or better than physician care in primary care settings, with no increase in adverse outcomes in FPA states.
How does Full Practice Authority improve healthcare access?
FPA allows NPs to serve as primary care providers in rural and underserved areas where physician shortages are common, reducing wait times and improving access to care.
Does Full Practice Authority lower healthcare costs?
Yes. FPA reduces administrative barriers and unnecessary oversight, leading to lower healthcare delivery costs while maintaining high-quality outcomes.
Can nurse practitioners open their own practices with FPA?
Yes. In FPA states, nurse practitioners can own and operate independent practices, expanding care access and creating leadership opportunities.
Why do some states still restrict NP practice?
Opposition often comes from concerns raised by physician organizations regarding training differences. However, evidence consistently supports NP safety, quality, and effectiveness.
How does Full Practice Authority impact patient satisfaction?
Patients treated by NPs report higher satisfaction due to longer visits, clearer communication, shorter wait times, and a stronger focus on education and prevention.
What does Full Practice Authority mean for NP career growth?
FPA enables NPs to lead care teams, innovate in telehealth and community care, specialize independently, and fully use their education and training.
Will Full Practice Authority become national?
Many experts predict broader adoption within the next 5–7 years, driven by healthcare shortages, federal initiatives, and positive outcomes in existing FPA states.
Key Definitions
Full Practice Authority (FPA)
A state-level policy that allows nurse practitioners to evaluate patients, diagnose conditions, order tests, and prescribe medications without physician supervision.
Nurse Practitioner (NP)
An advanced practice registered nurse with graduate-level education trained to provide primary and specialty care.
Advanced Practice Registered Nurse (APRN)
An umbrella term that includes nurse practitioners, certified nurse midwives, clinical nurse specialists, and nurse anesthetists.
Restricted Practice Authority
A practice model where NPs must work under physician supervision or collaborative agreements to provide care.
Reduced Practice Authority
A model where NPs can practice independently in some areas but still require physician involvement for certain tasks.
Primary Care Provider
A healthcare professional who delivers first-contact, continuous, and comprehensive patient care.
State Board of Nursing
The regulatory body that licenses and governs nursing practice within each state.
Occupational Licensing Requirements
State laws that define who can provide healthcare services and under what conditions.
Healthcare Access Gap
The lack of timely and affordable healthcare services, often affecting rural and underserved populations.
Patient-Centered Care
A care approach that prioritizes patient education, prevention, communication, and shared decision-making.
About the Author
- NPHub Staff
At NPHub, we live and breathe clinical placements. Our team is made up of nurse practitioners, clinical coordinators, placement advisors, and former students who’ve been through the process themselves. We work directly with NP students across the country to help them secure high-quality preceptorships and graduate on time with confidence. - Last updated
November 10th, 2025 - Fact-checked by
NPHub Clinical Placement Experts & Student Support Team - Sources and reference
- https://www.nphub.com/blog/why-nurse-practitioner-is-a-good-career-choice
- https://www.nphub.com/
- https://myamericannurse.com/primary-care-shortages-and-the-role-of-family-nurse-practitioners
- https://www.nphub.com/blog/5-ways-nurse-practitioners-improve-access-to-care
- https://www.nphub.com/blog/ways-nurse-practitioners-positively-impact-patient-outcomes
- https://www.nphub.com/blog/nps-vs-mds-unraveling-the-differences
- https://www.aanp.org/advocacy/advocacy-resource/position-statements/quality-of-nurse-practitioner-practice
- https://pubmed.ncbi.nlm.nih.gov/31607371/
- https://www.nphub.com/blog/choosing-the-right-nurse-practitioner-specialty-factors-to-consider
- https://www.nphub.com/blog/full-practice-authority-california-bill-ab-890
- https://www.nphub.com/blog/launch-np-private-practice-guide
Find a preceptor who cares with NPHub
Book a rotation.webp)







.webp)


.webp)


%20(3)%20(2).svg)
.webp)