TL;DR: Key Takeaways for Finding No-Cost NP Preceptor Solutions
- Yes, finding a free NP preceptor is possible but requires strategy, persistence, and organization.
- Leverage your nursing school’s practicum coordinators, faculty, and alumni networks as your first line of support.
- Use free online directories like the AANP NP Preceptor Knowledge Center and social media groups to identify potential preceptors.
- Combine cold outreach via email, phone, and in-person visits with consistent follow-up to maximize your chances.
- Stay organized by tracking all contacts, responses, and paperwork deadlines to avoid last-minute stress.
- Ready to streamline your outreach and keep everything in one place? Create your free NP Hub account today and take control of your clinical placement journey!
Start Here: Can You Really Find a Free NP Preceptor?
Yes, but it requires strategy, structure, and persistence.
The good news is that nurse practitioner students secure preceptors without paying matching fees every semester. The reality is that free solutions demand more effort, more organization, and more follow-through than their paid counterparts. This guide breaks down the specific no-cost tools—Facebook groups, professional directories, networking strategies, YouTube training, and more—that actually work when you use them with intention.
This isn’t vague “just network more” advice. You’ll find step-by-step approaches, real resources, and practical timelines designed to bring support, less stress, and a clear structure to your clinical placement process.
NP Hub specializes in preceptor matching and has helped students across the country connect with experienced preceptors. But this article is dedicated to walking you through every free option first, because we believe you deserve to understand all your choices before deciding what’s right for your situation.
If you want a central place to organize your outreach, track responses, and get guidance along the way, you can create a free NP Hub account to stay organized even while pursuing no-cost strategies.
Understanding the NP Preceptor Journey (And Why It Feels So Hard)
Completing your nurse practitioner program means logging somewhere between 500 and 1,000 clinical hours under the supervision of qualified healthcare providers. These clinical rotations aren’t just checkbox requirements—they’re where theoretical knowledge transforms into real patient care skills. You’ll develop assessment, diagnosis, and treatment abilities that no classroom simulation can replicate.
The challenge? Many NP programs—especially online and hybrid programs that have expanded rapidly since 2015—expect students to self-secure their own clinical sites. Your program might provide some guidance, but the responsibility often lands squarely on your shoulders.
The main pain points are predictable but still stressful:
- Tight deadlines that leave little room for last-minute scrambling
- Program-specific paperwork and site credentialing requirements
- High demand in popular specialties like family medicine, women’s health, pediatrics, and mental health
- Limited preceptor availability in competitive geographic areas
Beyond logistics, there’s an emotional toll. Many NP students feel alone and unsupported when their practicum coordinator can only offer limited help. The uncertainty of not knowing where you’ll complete your rotation creates anxiety that compounds over time.
Here’s the reassuring part: a structured plan changes everything. This guide moves from the lowest-effort, highest-leverage free strategies to more advanced, time-intensive ones. Follow it in order, and you’ll have a roadmap that reduces stress and keeps you on track.
BUTTON
Leverage Your School’s Built-In Support (Practicum Coordinators & Faculty)
No-cost preceptor solutions start at your nursing school, and many students underuse the resources already available to them.
Your practicum coordinator likely maintains lists of prior preceptors organized by specialty and location. These aren’t always advertised, so you’ll need to ask directly. Faculty members who supervise clinical education often have professional relationships with clinicians who regularly accept students.
Here’s how to maximize school support:
Request structured help. Ask your coordinator for:
- A written timeline of placement deadlines
- School-specific preceptor requirements and credentialing forms
- Sample outreach emails or call scripts that have worked for previous students
Explore institutional partnerships. Some programs have standing agreements with health systems, community health centers, or clinics that take student NP rotations at no cost. Your coordinator may not volunteer this information unless you ask.
Tap alumni networks. Graduates from your program who are now practicing NPs sometimes return as preceptors. Ask if your school maintains an alumni directory or can facilitate introductions.
Create a tracking system. Whether you use a spreadsheet or a free NP Hub account, document all school-provided leads with contact information, follow-up dates, and paperwork deadlines. This structure prevents leads from slipping through the cracks and reduces the mental load of managing multiple conversations.
Don’t assume your coordinator will proactively provide guidance. Be specific in your requests, and you’ll often find more support than you expected.
Using Free Online Directories and Knowledge Centers the Right Way
Online directories aren’t full matching services, but they can be powerful research tools when approached with a plan.
What the AANP NP Preceptor Knowledge Center Offers
The AANP NP Preceptor Knowledge Center is a credible professional resource maintained by the American Association of Nurse Practitioners. It includes educational materials like “Precepting with a Purpose: A Comprehensive Guide for Nurse Practitioner Preceptors,” designed to help practicing NPs understand best practices in clinical training.
Here’s what students need to understand: the AANP NP Locator Tool within this center is primarily patient-facing. It helps patients find a nurse practitioner by zip code—it’s not designed as a student tool for finding preceptors. There’s no indicator of whether a listed NP accepts students or is willing to serve as a clinical preceptor.
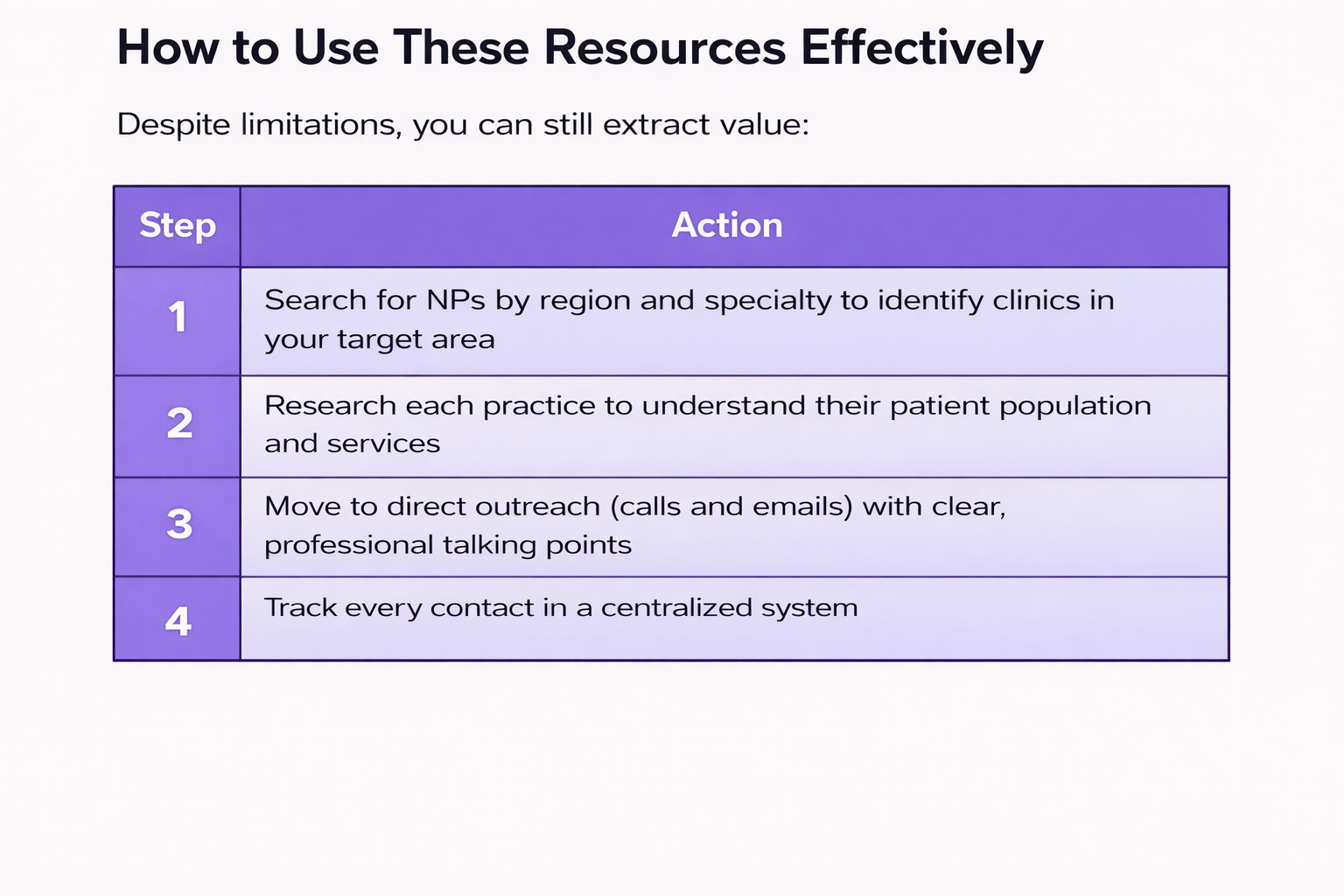
Remember that these resources provide names and starting points, not guaranteed acceptance or help with school paperwork. You bring the structure and persistence.
Consider combining directory leads with a free NP Hub account to store contacts, outreach dates, and responses in one organized location.
Facebook Groups and Social Media: Turning Communities into Preceptorships
Facebook groups and NP communities are currently some of the most active free spaces where students and potential preceptors connect directly.
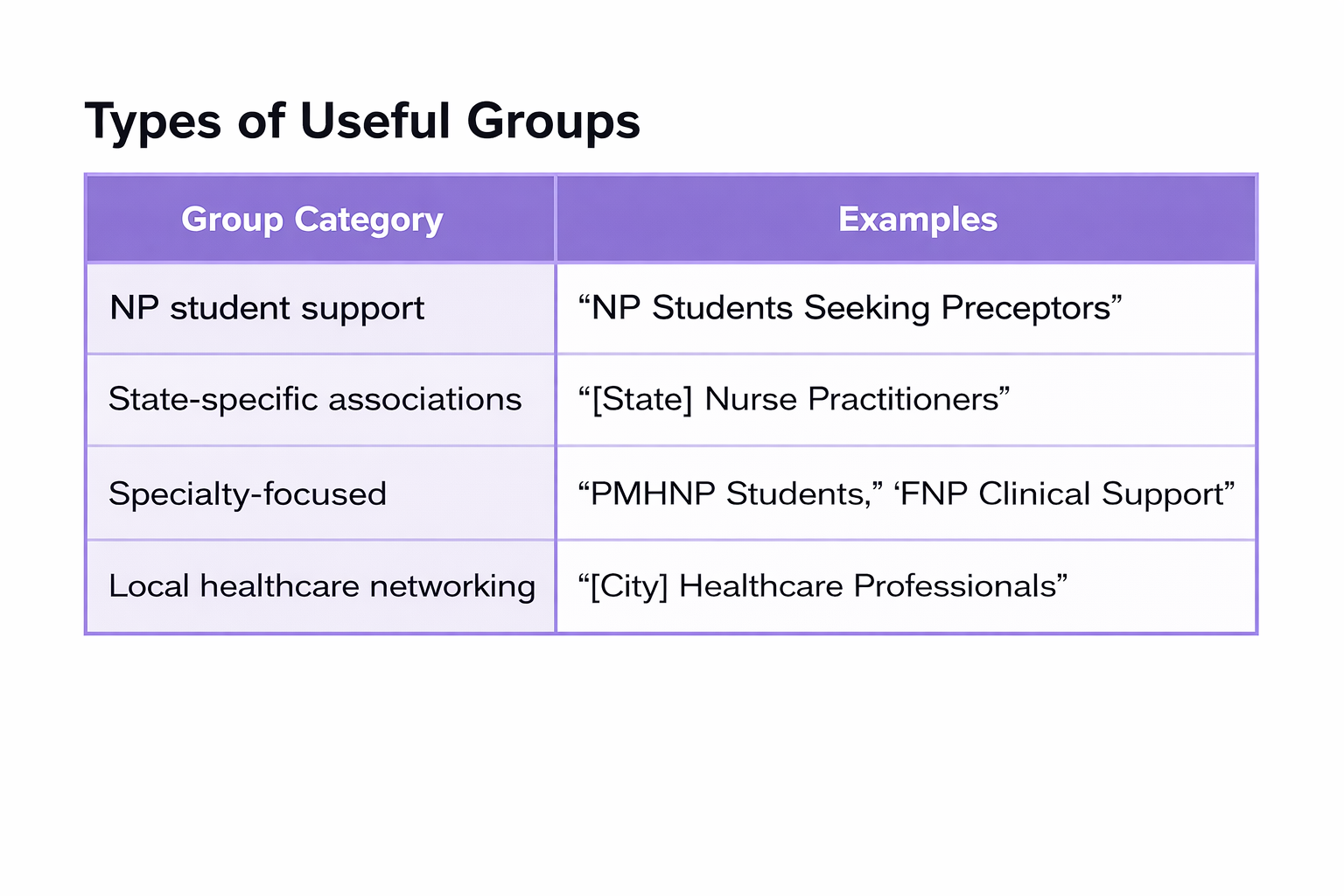
How to Find Relevant Groups
Search Facebook using specific terms:
- “nurse practitioner preceptor [your state]”
- “NP clinical rotations [your city]”
- “FNP students preceptor help”
- “[Specialty] nurse practitioner students”
Some groups have thousands of members, which means high visibility for your posts—but also high volume that can bury requests quickly.
Posting an Effective Preceptor Request
A clear, specific request dramatically increases your chances of getting responses. Include:
- Your program type (FNP, PMHNP, WHNP, AGPCNP, etc.)
- Expected graduation semester and year
- Specific rotation dates needed
- Location and how far you can travel
- Any flexibility (evenings, weekends, telehealth hours)To dramatically increase your chances of securing a preceptor, your initial outreach or request must be clear, professional, and highly specific. A vague request is often overlooked or dismissed.
Your request should thoroughly cover the following critical elements:1. Professional and Program Context
- Your Program Type and Specialization: Clearly state the specific Nurse Practitioner program you are enrolled in (e.g., Family Nurse Practitioner - FNP, Psychiatric Mental Health Nurse Practitioner - PMHNP, Women's Health Nurse Practitioner - WHNP, Adult-Gerontology Primary Care Nurse Practitioner - AGPCNP, etc.). This ensures the preceptor knows if their practice setting aligns with your educational requirements.
- Anticipated Graduation Timeline: Provide your expected graduation semester and year. This gives the preceptor an idea of your overall program progression and long-term goals.
2. Clinical Rotation Specifics
- Specific Rotation Dates Needed: Be precise with the required timeframe, including both the start and end dates of the rotation. Avoid saying "in the fall" and instead use "September 4, 2026, to December 15, 2026."
- Required Clinical Hours: State the exact number of clinical hours mandated by your program for the specific rotation (e.g., "I require 180 clinical hours for this primary care rotation").
3. Location and Logistics
- Preferred Location and Travel Radius: Clearly indicate the city, state, or general geographic area where you are seeking the placement. More importantly, specify how far you are willing to travel from your home base (e.g., "Seeking placement in the greater Seattle area; I am able to travel up to a 60-mile radius from Tacoma").
4. Flexibility and Schedule
- Availability for Non-Traditional Hours: Highlight any flexibility you have, as this can make you a more appealing student. Mention your willingness to commit to:
- Evenings: Availability past standard 9-to-5 hours.
- Weekends: Openness to Friday evenings, Saturdays, or Sundays.
- Telehealth Experience and Capability: If your program allows for remote clinical hours, state your capacity and willingness to participate in supervised telehealth sessions, as this can significantly expand the potential preceptor pool.
- Required clinical hours for this rotation
Group Etiquette That Gets Results
- Follow group rules carefully—many have specific posting formats
- Offer to share your resume or CV in messages
- Avoid spamming multiple posts in the same week
- When someone comments or likes your post, follow up politely via Messenger
- Thank members who respond, even if they can’t help directly

Practical Tips to Make Social Media Outreach Actually Work
Keep posts short and professional. Include a photo and a one-sentence introduction about who you are and what rotation you need. This builds trust quickly and makes you memorable in a sea of text-only requests.
Search group archives strategically. Use keywords like “preceptor,” “clinical site,” or “rotation” to find older posts. Members who previously offered help may still be available—reach out directly via private message.
Use LinkedIn in parallel. Optimize your headline to read something like “MSN-FNP Student Seeking Preceptor in [City, State] – Spring 2026” and connect with NPs, PAs, and MDs in your area. Many healthcare professionals are more active on LinkedIn than Facebook.
Combine online and offline networking. Success on social media increases significantly when you pair it with in-person connections through work colleagues, local providers, or professional events. Social media works best as one tool in a larger strategy, not a stand-alone tactic.
If social media leads stall after a few weeks of consistent effort, NP Hub can provide guidance and next steps through a free account designed to keep you on track.
Free NP Preceptor Finder Articles, Videos, and Tool Roundups
Some of the most helpful no-cost resources aren’t tools at all—they’re in-depth guides and videos that show real outreach strategies and scripts you can adapt.
NP Hub’s Free Educational Content
NP Hub has published extensive free guides specifically for students navigating preceptor challenges:
Find Free Preceptors Guide – This walkthrough covers practical, real-world approaches including what to say in outreach emails, how to follow up without being pushy, and when to try different tactics.
Free NP Preceptor Finder Tools Review – This resource breaks down which free tools are worth your time and which are just static lists with outdated information. It helps you set the record straight about what these tools can and cannot do.
Video Walkthroughs
Sometimes reading isn’t enough—watching someone demonstrate the process makes it click.
YouTube: The Ultimate Free NP Preceptor Finder – This video provides a visual, less stressful way to learn outreach strategies, showing real examples of posts and follow-up emails.
YouTube: Building Your Placement Timeline – Covers topics like reducing stress, understanding school requirements, and creating a realistic schedule for your clinical placement process.
Study these resources first, then use them as templates for your own outreach plan. This reduces guesswork and provides the structure most students feel is missing from their programs.
Why “Free Tools” Alone Aren’t a Full Strategy
Let’s set realistic expectations: most free NP preceptor finder tools are directories, lists, or discussion threads. They rarely confirm availability, verify credentials, or handle documentation.
The limitations are significant:
- No real-time updates on which preceptors are currently taking students
- No specialty or location filters in many cases
- No support for required paperwork or compliance
- No backup options if a preceptor cancels
These limitations mean that relying solely on free NP preceptor finder tools can leave students vulnerable to unexpected challenges. Without current information on preceptor availability, students may spend valuable time pursuing leads that have already closed to new learners. The absence of specialty or geographic filters further complicates the search, especially for those needing specific clinical experiences within a manageable travel distance.
Moreover, free tools rarely assist with the essential administrative tasks such as completing school paperwork, verifying credentials, or ensuring site compliance, all of which are critical to securing a valid clinical placement. When a preceptor unexpectedly cancels or becomes unavailable, free tools typically provide no contingency plans or alternative options, leaving students scrambling to find last-minute replacements.
Because of these gaps, nurse practitioner students must approach free preceptor finders as just one part of a broader, proactive strategy. Combining these tools with personal networking, direct outreach, and organized follow-up increases the likelihood of successfully securing a no-cost preceptor and completing clinical rotations on time.
Relying solely on free finders can lead to last-minute panic when your rotation is 2-3 months away and no site is confirmed. Delayed graduation, additional tuition costs, and missed clinical hour deadlines become real risks.
Treat free tools as phase one: research and lead generation. They’re the starting point of your personalized matching process, not the complete solution from start to finish.
NP Hub’s free resources and account dashboard can help you recognize when it’s time to escalate from free tools to more hands-on support if your timeline is at risk.
Why Rural Health Clinics Are a Hidden Gem for No-Cost NP Preceptor Opportunities
Rural health clinics often have lower competition and higher needs for assistance, making them more receptive to students. These clinics typically serve underserved populations and may have fewer resources, which increases their willingness to accept nurse practitioner students eager to contribute to patient care. Additionally, rural clinics often face staffing shortages, so having motivated students can help ease the workload while providing valuable learning experiences.
Students who pursue clinical rotations in rural settings benefit from exposure to a broad range of conditions and a more hands-on role in patient management due to the smaller healthcare teams. This environment not only enriches clinical education but also fosters strong professional relationships and community engagement.
When reaching out to rural clinics, it’s important to highlight your flexibility and eagerness to learn, as well as your commitment to supporting their patient population. Demonstrating an understanding of the unique challenges rural healthcare providers face can make your request more compelling. Furthermore, rural clinics may be more open to accommodating telehealth clinical hours, which can expand opportunities for students who cannot relocate.
Overall, targeting rural health clinics as part of your no-cost NP preceptor search strategy can increase your chances of finding a receptive preceptor while gaining diverse and impactful clinical experience.
Networking, Cold Outreach, and Local Connections—Still 100% Free
The highest-yield no-cost preceptors often come from personal or local connections, even when that starts with a cold email or phone call.
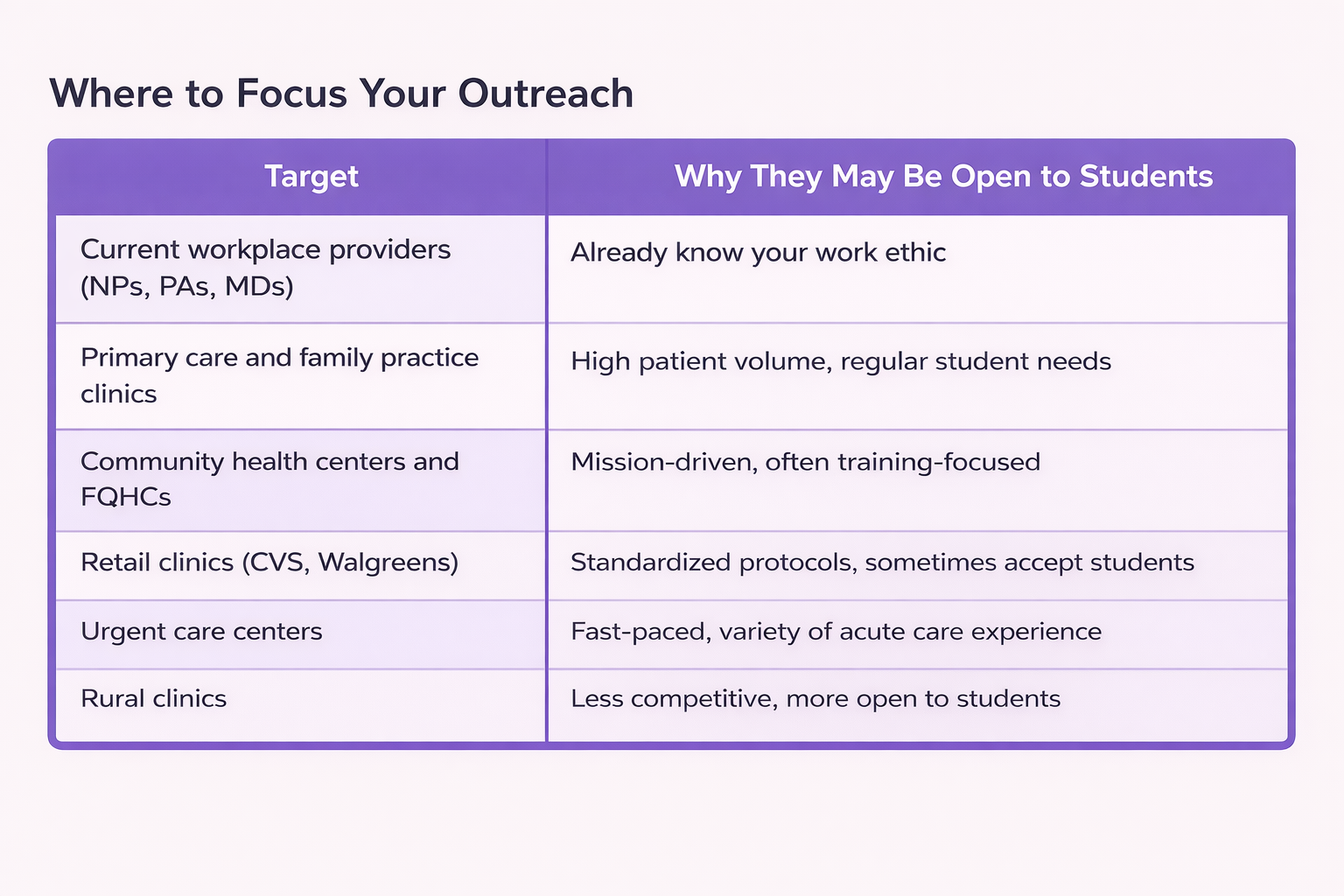
A Structured Outreach Process
- Make a list of 30-50 clinics within your defined travel radius
- Gather contact information, especially for office managers
- Schedule blocks of time each week dedicated to outreach
- Track every contact: name, date, response, and follow-up date
When you reach out, be professional and specific. Explain what rotation you need, your school’s name, exact dates, and required hours. Ask directly: “Does anyone in your practice accept NP students for clinical rotations?”

Cold Calling vs. Email vs. In-Person Visits
Email first is often the best approach. Office managers can discuss your request with providers without putting anyone on the spot. Include your CV, rotation request details, and a clear subject line.
Phone calls work well for confirming the right contact person and following up on emails. Prepare a short script:
“Hi, I’m [Name], a nurse practitioner student at [School]. I’m looking for a [specialty] preceptor for [dates]. I emailed last week and wanted to follow up. Could you direct me to the right person to discuss this?”
In-person visits can work in smaller practices or rural settings where relationships matter more than formal processes. Be respectful of clinic flow—avoid peak hours, keep it brief, and bring your CV to leave behind.
Persistence matters. Polite follow-up every 7-10 days can be the difference between a missed opportunity and a confirmed preceptor. Most students who struggle with cold calling give up too soon. Many clinicians are busy, not uninterested—sometimes your third message is the one they finally have time to answer.
If cold outreach feels overwhelming, NP Hub’s educational blogs and videos can serve as a virtual coach for messaging and timing strategies.
Free Support From NP Hub: Education, Orientation, and Backup Options
While NP Hub specializes in paid np preceptor matching, the company invests heavily in free education and orientation for nurse practitioner students at every stage of their journey.
Recognition From NP Programs Nationwide
Many universities now recognize the value of organized, structured support for students navigating clinical placements. The article on preceptor matching recommended by schools nationwide explains why programs are increasingly endorsing streamlined process approaches that reduce stress and improve outcomes.
Free YouTube Content
NP Hub’s YouTube channel includes videos like this walkthrough covering:
- Building a realistic placement timeline
- Understanding what your school actually requires
- Reducing anxiety through preparation
- Knowing when free strategies are working and when to adjust
Your Free NP Hub Account as a Control Center
A free NP Hub account can function as your central dashboard throughout the placement process:
- Access guides and educational content
- Track your outreach attempts and responses
- Understand when to shift from free options to more robust assistance
- Get oriented on what preceptor information your school needs
The goal isn’t to push you toward paid services—it’s to ensure you graduate on time with less anxiety, whether you find a preceptor through free methods or eventually need additional support.
Things to Avoid When Securing Preceptor Non-Cost Agreements
When establishing relationships with preceptors that do not involve a direct financial cost, it is crucial for institutions to navigate the process with care to ensure the partnership is sustainable, compliant, and mutually beneficial. Avoiding the following pitfalls can significantly increase the success rate and longevity of these crucial clinical affiliations:I. Communication and Expectation Mismanagement
A. Vague or Undocumented Expectations:
- Avoid: Relying solely on verbal agreements or informal understandings regarding the preceptor's duties, the student's responsibilities, or the required time commitment.
- Why: Ambiguity leads to misinterpretations, resentment, and potential non-compliance with programmatic requirements.
- Instead: Always formalize the relationship with a written, mutually signed agreement that clearly defines roles, expected hours, student evaluation criteria, and the preceptor's authority and scope of instruction.
B. Ignoring Preceptor Workload and Capacity:
- Avoid: Overloading a preceptor with too many students simultaneously, or requesting commitments that significantly detract from their primary professional responsibilities.
- Why: This can lead to preceptor burnout, superficial student supervision, and a decline in the quality of the clinical experience, ultimately risking the end of the affiliation.
- Instead: Regularly assess the preceptor's capacity and schedule, offering a reasonable ratio of students to the preceptor's availability and clinical setting demands.
C. Lack of Clear Institutional Support:
- Avoid: Failing to provide clear points of contact, prompt responses to preceptor questions, or readily accessible resources (e.g., student handbooks, orientation materials, IT support).
- Why: Preceptors who feel unsupported or isolated are less likely to continue the partnership.
- Instead: Designate a dedicated clinical coordinator or faculty liaison for the preceptor, ensuring all necessary institutional resources and contact information are provided at the outset.
II. Administrative and Compliance Oversights
A. Skipping Necessary Onboarding and Credentialing:
- Avoid: Assuming a preceptor is ready to start without verifying their professional licensure, required certifications, or completing necessary institutional background checks or credentialing processes.
- Why: This can expose the institution and the student to significant liability and violate accreditation standards or state regulations.
- Instead: Implement a streamlined but mandatory onboarding process that ensures all preceptors meet institutional and regulatory requirements before a student begins placement.
B. Failure to Maintain Adequate Liability Coverage:
- Avoid: Not confirming that both the institution's liability insurance (covering the student) and the preceptor's professional liability coverage are current and appropriate for the clinical activities.
- Why: In the event of an incident, inadequate coverage can result in significant legal and financial consequences for all parties involved.
- Instead: Explicitly outline the liability coverage provided by the institution for the student in the affiliation agreement and verify the preceptor's coverage details.
C. Neglecting the Affiliation Agreement Renewal Process:
- Avoid: Allowing formal affiliation agreements to expire without a timely renewal or amendment process.
- Why: An expired agreement means the clinical rotation may be operating without a formal legal framework, creating compliance issues and potential risk.
- Instead: Establish a robust tracking system to monitor agreement expiration dates and initiate the renewal or re-evaluation process well in advance.
III. Neglecting the Non-Cost Value Proposition
A. Providing Insufficient or Unvalued Incentives:
- Avoid: Offering minimal "non-cost" perks that hold little practical value to the preceptor (e.g., outdated reading materials, generic thank-you notes without substance).
- Why: Even without payment, preceptors need to feel their time and expertise are genuinely appreciated and compensated through meaningful non-monetary benefits.
- Instead: Focus on high-value, non-cost incentives such as continuing education credits (CEUs), free access to institutional libraries/databases, faculty appointment titles, or professional development workshops.
B. Treating Preceptors as Passive Assets:
- Avoid: Failing to seek and incorporate feedback from preceptors about the students, the curriculum, or the overall clinical placement process.
- Why: Preceptors are clinical experts. Ignoring their input can lead to a stagnation of the program's quality and make the preceptor feel like an unvalued resource.
- Instead: Create formal mechanisms (e.g., surveys, annual meetings, check-ins) to solicit constructive criticism and actively demonstrate how their feedback is used to improve the program.
C. Disregarding the Relationship Aspect:
- Avoid: Treating the preceptor relationship strictly as a transactional arrangement that only requires contact when a placement is needed.
- Why: Long-term, sustainable affiliations are built on relationships. Neglecting communication outside of placement cycles weakens loyalty.
- Instead: Maintain regular, brief, professional communication throughout the year, acknowledging holidays, significant achievements, or sending relevant program updates to foster a sense of belonging to the academic community.
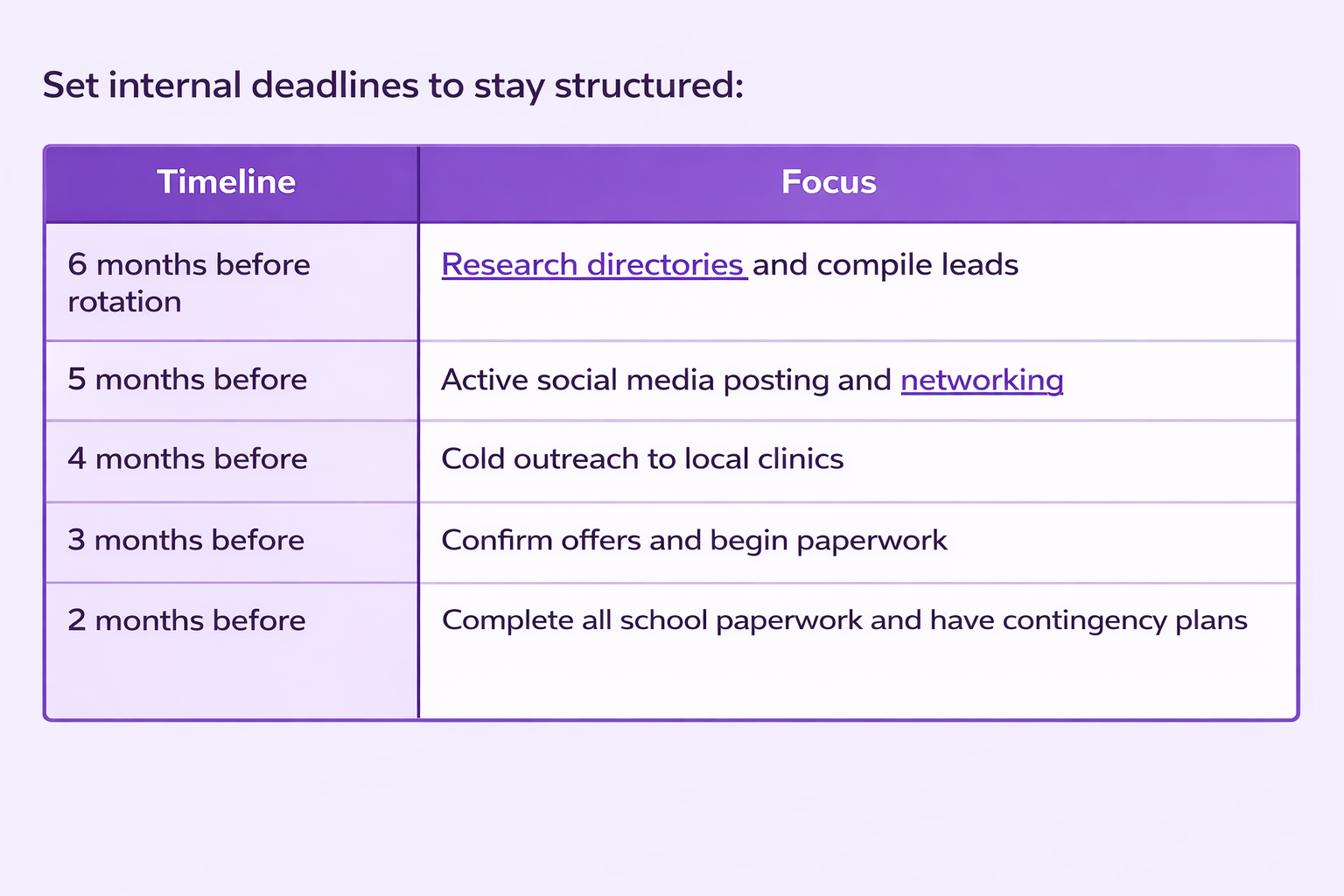
Putting It All Together: A Structured, No-Cost Game Plan
Finding preceptors without paying matching services is absolutely possible when you combine multiple approaches strategically. Use your school resources, AANP tools, Facebook groups, LinkedIn networking, local cold outreach, and NP Hub’s free content together—not as isolated attempts.
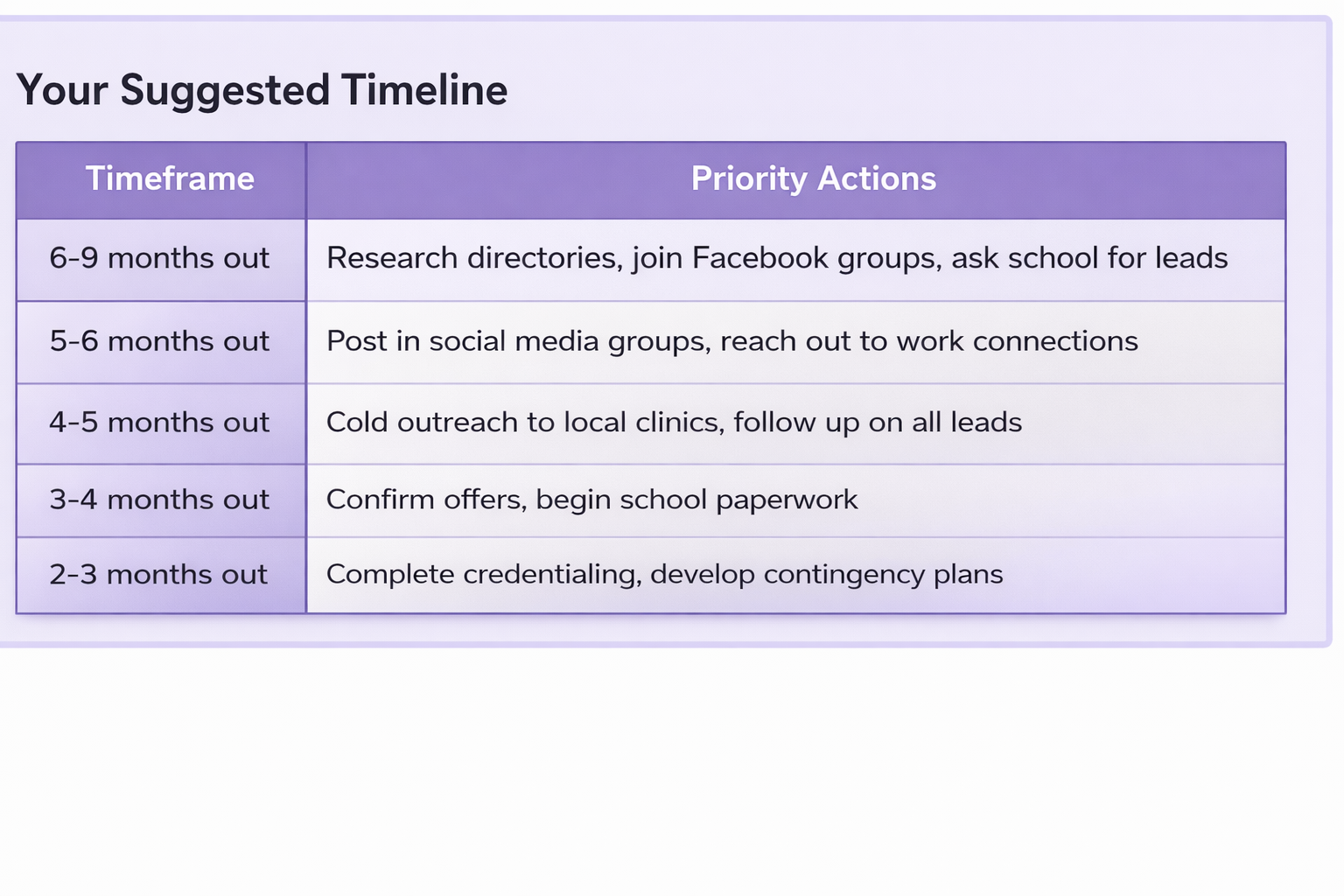
The difference between constant panic and a more peaceful clinical journey is structure, documentation, and realistic milestones—not just luck.
Stay Organized
To effectively track your efforts in securing NP preceptor solutions, it is essential to use at least one centralized system, such as a spreadsheet detailing the clinic name, contact information, date reached, response, and next steps, or a planner outlining your weekly outreach goals.
Reducing mental load through organization is one of the most effective ways to decrease stress throughout this fulfilling clinical experience.

You’re Not Alone
Thousands of NPs before you have navigated this exact process. Some found their perfect preceptor through a Facebook post. Others cold-called 30 clinics before one said yes. Many started with free strategies and later used matching services when timelines got tight.
There’s no single right path—only the path that gets you to graduation with your clinical hours complete and your sanity intact.
Help is available at every step, whether that’s free educational content, community support, or more hands-on placement requests assistance. The next generation of nurse practitioners will face the same challenges, and by learning this process, you’re building skills that serve patients for your entire career.
Start with the strategies in this guide. Track your progress. Ask for help when you need it. And remember: structure creates calm, persistence creates results, and support is always within reach.
Take the shortcut to graduation: Create your free NP Hub account now.
Key Definitions
Nurse Practitioner (NP) Preceptor:
A licensed healthcare professional, often an experienced nurse practitioner, physician assistant, or physician, who supervises and mentors NP students during their clinical rotations.
Clinical Rotations:
Hands-on training periods where NP students gain practical experience by working under the supervision of a preceptor in various healthcare settings.
Clinical Placement Process:
The series of steps NP students follow to secure a clinical site and preceptor for their required clinical hours, including outreach, paperwork, and approvals.
Preceptor Matching Services:
Organizations or platforms that connect NP students with available and qualified preceptors, often assisting with paperwork and coordination for a fee.
No-Cost NP Preceptor Solutions:
Strategies and resources that allow NP students to find preceptors without paying matching fees, typically involving personal outreach, school resources, and free online tools.
Frequently Asked Questions (FAQs)
Q: Can I really find a free NP preceptor without paying any fees?
A: Yes, it is possible to find a no-cost NP preceptor, but it requires persistence, strategic outreach, and effective organization. Utilizing school resources, networking, and free online directories can help you secure a preceptor without fees.
Q: When should I start looking for my NP preceptor?
A: It is recommended to begin your search at least 6 to 9 months before your clinical rotation starts. Early planning helps avoid last-minute stress and increases your chances of finding the right preceptor.
Q: What if my nursing school does not assign preceptors?
A: Many NP programs expect students to self-secure their clinical sites. In this case, leverage your practicum coordinator, alumni networks, professional associations, social media, and cold outreach to clinics and providers.
Q: Are paid preceptor matching services unethical?
A: No. Using paid services is a common and accepted practice as long as your program approves the preceptor and clinical site. Paid services often provide verified preceptors and handle paperwork, reducing stress.
Q: What specialties are hardest to find preceptors for?
A: High-demand specialties such as family medicine, women’s health, pediatrics, and mental health often have limited preceptor availability, especially in competitive geographic areas.
Q: How can I increase my chances of a preceptor accepting me?
A: Personalize your outreach messages, be professional, clearly state your rotation requirements, and follow up consistently. Highlight your strengths and flexibility to stand out among other students.
Q: What should I do if a preceptor cancels last minute?
A: Have contingency plans in place by maintaining a list of backup preceptors and continuing outreach even after securing a placement. Some matching services also offer support if cancellations occur.
Q: Can social media help me find a preceptor?
A: Yes, platforms like Facebook and LinkedIn can be valuable for networking with healthcare providers and NP students. Use targeted groups and professional connections to identify potential preceptors.
Q: How important is organization during the preceptor search?
A: Extremely important. Tracking contacts, responses, follow-up dates, and paperwork deadlines helps you stay on top of your search and reduces stress during the clinical placement process.
About the author
NPHub Staff
At NPHub, we live and breathe clinical placements. Our team is made up of nurse practitioners, clinical coordinators, placement advisors, and former students who’ve been through the process themselves. We work directly with NP students across the country to help them secure high-quality preceptorships and graduate on time with confidence.
Last updated
January 21st, 2026
Fact-checked by
NPHub Clinical Placement Experts & Student Support Team
Sources and references
https://www.nphub.com/testimonials
https://student.nphub.com/search
https://www.wocn.org/become-a-woc-nurse/preceptor-directory/
https://www.nphub.com/blog/rural-nurse-practitioners
https://www.youtube.com/watch?v=cMyx4m_awyY
https://www.youtube.com/watch?v=k7oR8kUPYnI
https://www.nphub.com/blog/preceptor-matching-recommended-by-schools-nationwide
https://www.youtube.com/@NPHub/videos
Find a preceptor who cares with NPHub
Book a rotation.webp)








.webp)


.webp)


%20(3)%20(2).svg)
.webp)