TL;DR: Summary
- NPs in Virginia earn competitive salaries, typically ranging from $120,000 to over $180,000 in major cities like Alexandria and Richmond, depending on experience and location.
- Your skills are most needed in Richmond, Virginia Beach, Norfolk, and Alexandria, offering diverse practice settings.
- Start early, leverage school resources, and be proactive in building personal connections to secure your clinical placements.
- Experienced PMHNPs can apply for autonomous practice in Virginia as of July 1, 2024, without a physician agreement.
- Accredited programs, like UVA's CCNE-accredited PMHNP program, require a minimum of 504 clinical hours and lead to ANCC certification eligibility.
- Comprehensive support, including scholarships and grants, is available to help fund your PMHNP education.
- Ready to streamline your clinical placement search? Open your free NPHub account today to connect with top preceptors and secure your required clinical hours.
Embarking on your journey to become a Psychiatric Mental Health Nurse Practitioner (PMHNP) in Virginia is both exciting and filled with important choices. Most PMHNP pathways begin with a bachelor’s degree program, specifically a Bachelor of Science in Nursing (BSN), which is required for admission to most graduate nursing programs. Understanding the landscape—from finding the right preceptor to knowing where your career opportunities lie—can empower you to make decisions that align with your goals, values, and emotional well-being. This guide is designed to support you with transparency, trust, and respect for your autonomy every step of the way.
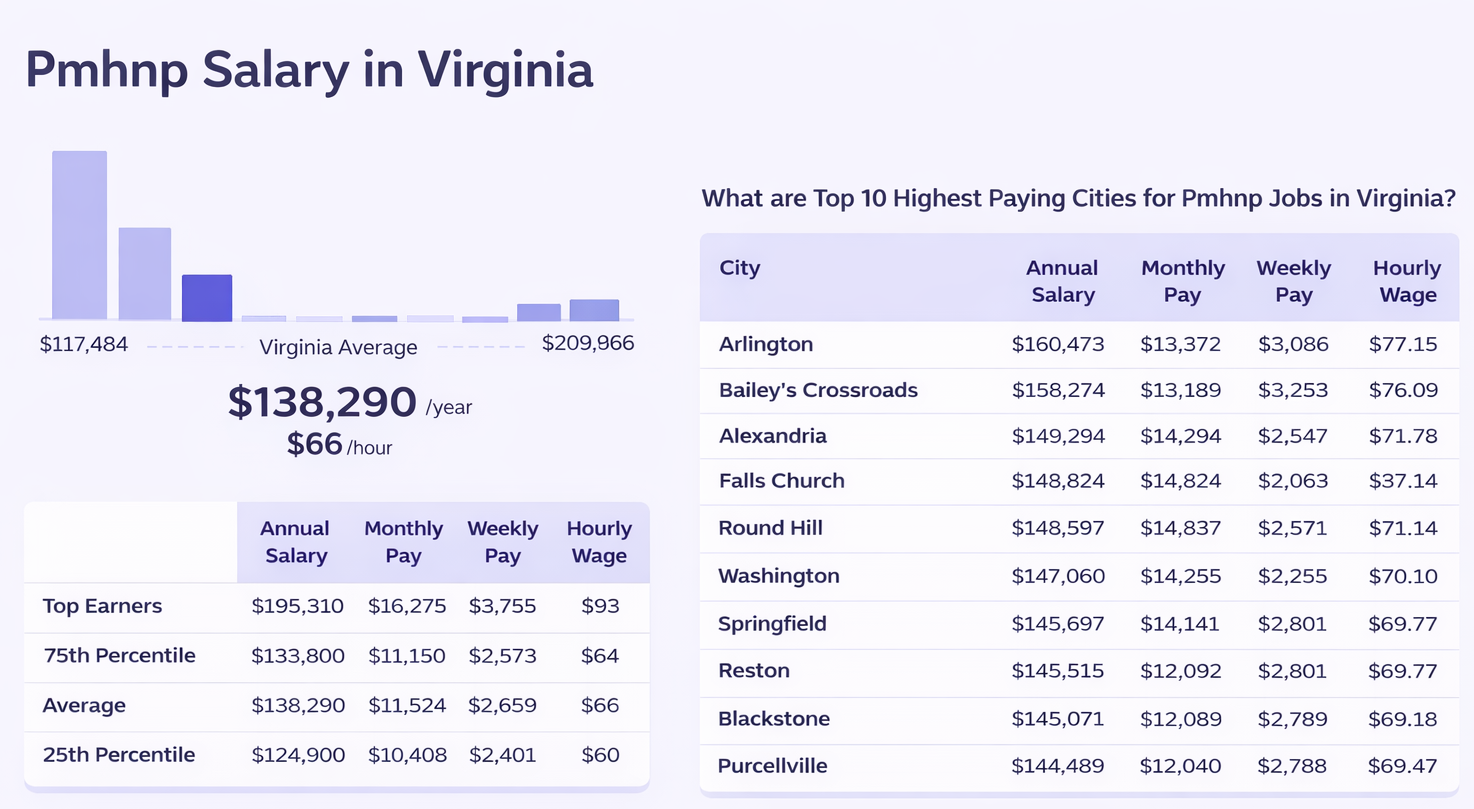
How Much Can a Nurse Practitioner Earn in Virginia?
Your future as a Nurse Practitioner (NP) in Virginia holds promising financial potential, especially in key urban areas where demand for mental health care is strong. Here’s a snapshot of what you might expect, keeping in mind that salaries can vary based on experience, setting, and specialization:
- Richmond: As the state capital, Richmond offers competitive salaries for PMHNPs, often ranging from $120,000 to $160,000 annually. The city blends urban living with a supportive healthcare community.
- Virginia Beach: Known for its diverse population and military presence, NPs here can expect salaries typically between $115,000 and $155,000, with opportunities in both hospitals and community clinics.
- Norfolk: With a growing healthcare sector, Norfolk provides salaries in a similar range to Virginia Beach, often coupled with a strong network of veteran and military healthcare services.
- Alexandria and Arlington: These areas near Washington, D.C., offer some of the highest salary ranges, from $130,000 up to $180,000 or more, reflecting the high cost of living and demand for specialized mental health services.
Employment opportunities and compensation for PMHNPs in Virginia vary by location and experience, with salaries typically ranging from approximately $120,000 to over $220,000 annually.
Choosing your practice location is a balance between financial goals and lifestyle preferences. Urban centers offer higher salaries but may come with a faster pace and higher living costs, while smaller cities or suburban areas can provide a more relaxed environment with meaningful patient connections.
Cities in Virginia with the Most Nurse Practitioner Opportunities
If you're seeking areas where your expertise will be highly valued, certain cities frequently have a strong demand for Nurse Practitioners, particularly those specializing in psychiatric mental health:
Each city offers unique practice settings—from large hospital systems and outpatient clinics to private practices and community health centers—allowing you to find an environment that resonates with your personal and professional aspirations.
Securing Clinical Preceptors in Virginia: A Student’s Guide
Finding the right preceptor is a crucial step in your PMHNP education, as this relationship shapes your clinical experience and confidence. Here’s how to approach this process with control and clarity:
- Start Early and Be Proactive: Begin identifying potential preceptors well before your clinical rotations. Students are encouraged to begin to identify potential clinical sites for these experiences prior to the beginning of the program. This gives you time to build relationships and ensures you can choose a preceptor who aligns with your learning style and career goals.
- Leverage Your School’s Resources: Many nursing programs have established networks and coordinators who assist with clinical placements. Clinical placements for PMHNP programs are often arranged by faculty who work to locate appropriate sites and preceptors. Use these resources as a starting point, but remember that you have the final say in selecting a preceptor who feels like the right fit.
- Consider Your Practice Preferences: Think about the patient populations, practice settings, and types of psychiatric care you want to experience. Clinical rotations in PMHNP programs include experiences with child/adolescent and geriatric populations, as well as adult inpatient and outpatient care, and these experiences take place in a variety of clinical settings. Communicate these preferences clearly when reaching out to potential preceptors.
- Build a Personal Connection: When contacting preceptors, be genuine about your goals and eager to learn. A respectful and transparent approach can foster trust and open doors.
- Understand the Logistics: Ensure that your preceptor is licensed and approved by your program and the Virginia Board of Nursing to supervise clinical hours. Confirm the number of hours they can accommodate and their availability.
Many students find potential employment opportunities at their clinical placement sites upon graduation, helping to prepare them for their future role.
Emotional Benefit: Taking charge of your preceptor selection helps you feel supported and confident, reducing stress and building a foundation for a meaningful clinical experience.
Many nursing programs prefer or require at least one year of direct patient care experience for admission.
Associations and Communities for Nurse Practitioners in Virginia
Connecting with professional associations can enrich your journey by providing mentorship, educational resources, and networking opportunities. Some valuable organizations include:
- Virginia Nurses Association (VNA): Offers advocacy, continuing education, and a community of nurses across specialties.
- Virginia Council of Nurse Practitioners (VCNP): Focuses on advancing NP practice and provides resources tailored to nurse practitioners in Virginia.
- American Psychiatric Nurses Association (APNA): A national organization with a strong Virginia presence, offering specialized support for psychiatric nurses.
- National Alliance on Mental Illness (NAMI) Virginia: While not exclusive to nurses, NAMI provides community engagement and advocacy opportunities related to mental health.
Joining these groups can help you stay informed about legislative changes, access job postings, and find mentors who understand your unique challenges.
Understanding Nurse Practitioner Law in Virginia
According to the Virginia Board of Nursing Regulations, Virginia’s laws shape how you will practice as a PMHNP, so knowing them empowers you to navigate your career confidently. APRN education is a comprehensive program that prepares nurses for advanced clinical and leadership roles:
- Practice Agreements: Until recently, NPs in Virginia were required to have a collaborative practice agreement with a physician. However, as of July 1, 2024, experienced PMHNPs with at least 3 years (or 5,400 hours) of full-time clinical experience may apply for autonomous practice, allowing you to operate independently. Virginia law allows physicians to enter into a practice agreement with up to 10 PMHNPs at one time.
- Prescriptive Authority: PMHNPs in Virginia have the authority to prescribe Schedule II through Schedule VI controlled substances, supporting comprehensive psychiatric care.
- Licensure Requirements: To practice, you must hold an active RN license, complete an accredited PMHNP program (MSN or DNP), pass the national certification exam through the American Nurses Credentialing Center (ANCC), and obtain licensure through the Virginia Board of Nursing. To apply for APRN licensure, documentation of advanced degree, national certification, and a background check is required. After graduating, one must apply for an Advanced Practice Registered Nurse (APRN) license through the Virginia Board of Nursing. PMHNPs must maintain a valid, unrestricted license from the Virginia Board of Nursing to practice. To obtain Registered Nurse (RN) Licensure, one must pass the NCLEX-RN and hold a current, active, and unencumbered RN license in Virginia or a compact state.
- Continuing Education: Maintaining your license requires ongoing education and adherence to state regulations to ensure safe, current practice.
Students must maintain current licensure throughout their PMHNP program, and additional RN licenses may be necessary for clinical rotations.
Understanding these laws helps you feel secure and prepared to advocate for your professional autonomy and the care your patients deserve.
Independent Practice and Billing for PMHNPs in Virginia
Psychiatric Mental Health Nurse Practitioners (PMHNPs) in Virginia have the opportunity to operate independently after meeting specific state requirements. This means that experienced PMHNPs can run their own private practices, providing comprehensive mental health care without the need for physician oversight.
Independent practice allows PMHNPs to directly bill patients and insurance providers for their services, enhancing their professional autonomy and expanding access to mental health care. This capability supports a more streamlined patient experience and enables PMHNPs to tailor treatment plans and follow-ups efficiently.
To qualify for autonomous practice, PMHNPs must complete at least three years or 5,400 hours of full-time clinical experience. Once eligible, they can fully utilize their prescriptive authority, including prescribing controlled substances, and manage complex care in various settings.
This shift toward independent practice reflects the growing recognition of PMHNPs as vital providers in addressing mental health disorders and improving community well-being across Virginia.
Financial Aid and Support for PMHNP Students in Virginia
Pursuing a Psychiatric-Mental Health Nurse Practitioner (PMHNP) degree at the regionally accredited University of Virginia School of Nursing prepares advanced practice nurses to diagnose and manage mental health conditions across the lifespan.
The University of Virginia offers comprehensive financial aid—including scholarships, grants, and loans—for both on-campus and online students, with personalized guidance to reduce financial stress.
Students benefit from robust academic advising, counseling, and mentorship from experienced faculty, helping them build strong diagnostic skills and prescriptive authority. The PMHNP program emphasizes clinical experience, including a minimum of 504 clinical hours in diverse settings like psychiatric hospitals and community health organizations, vital for practical skills in assessing varied populations (children, families, adults).
Accredited by the CCNE, the curriculum includes 14 credit hours of core courses. Graduates are eligible for the ANCC certification exam, opening doors to advanced PMHNP roles. A doctoral degree prepares graduates for leadership, policy development, and potentially higher salaries. The program's strong focus on clinical experience, academic support, and financial aid makes it an excellent choice for those committed to mental health care.
Your journey as a PMHNP student in Virginia is uniquely yours. By understanding your options, laws, and resources, you can create a fulfilling, balanced path that supports both your professional ambitions and emotional well-being. Remember, you are in control of your education and career—choose what feels right for you.
Frequently Asked Questions (FAQ)
Q: How do I find a preceptor if my school doesn’t provide one?
A: Start by reaching out to local clinics, hospitals, and mental health centers. Use professional associations and networking events to connect with potential preceptors. Always communicate your goals and ensure their credentials meet your program’s requirements.
Q: Can I practice independently as a PMHNP in Virginia right after graduation?
A: Not immediately. You need at least 3 years or 5,400 hours of full-time clinical experience before applying for autonomous practice without a physician agreement.
Q: What types of settings do PMHNPs work in Virginia?
A: PMHNPs practice in hospitals, outpatient clinics, private practices, schools, residential substance abuse facilities, nursing homes, and the Department of Veterans Affairs, among others.
Q: Are there online resources to help with clinical placements?
A: Many programs offer online portals and coordinators to assist with placements. Additionally, professional associations often list clinical opportunities and preceptor directories.
Key Definitions
- PMHNP (Psychiatric Mental Health Nurse Practitioner): An advanced practice nurse specializing in mental health care across the lifespan.
- Preceptor: An experienced practitioner who supervises and mentors nursing students during clinical rotations.
- Prescriptive Authority: The legal ability to prescribe medications, including controlled substances.
- Autonomous Practice: The ability to practice independently without physician oversight.
- Clinical Hours: The supervised practical experience required to complete a nursing program.
- Credit Hour: A unit representing the amount of coursework or clinical experience required, used to measure academic progress in nursing programs.
- DNP Program (Doctor of Nursing Practice Program): An advanced nursing degree program focused on clinical expertise, leadership, and evidence-based practice, preparing nurses for the highest levels of nursing practice and leadership roles.
- Nursing Practice: The professional responsibilities and activities of nurses, especially at the advanced level, including leadership, clinical decision-making, and specialized care.
- Online Coursework: Virtual classes and assignments accessible remotely, allowing students to complete program requirements with flexibility.
- Online Students: Students enrolled in online programs who access coursework and resources virtually, often balancing studies with personal and professional commitments.
- Person: The individual receiving person-centered mental health care, with a focus on holistic and personalized treatment.
- Psychology: The study of mind and behavior, relevant to mental health nursing for understanding patient needs and applying research methods.
- Review: The process of assessing or verifying clinical or program information, such as reviewing laws, assessment data, or clinical models.
- Management: The evidence-based management of mental health disorders, including assessment, diagnosis, and treatment planning for individuals across the lifespan.
- American Nurses Credentialing Center (ANCC): The organization that certifies nurse practitioners nationally.
- Virginia Board of Nursing: The regulatory body overseeing nursing licensure and practice in Virginia.
About the Author
- NPHub Staff
At NPHub, we live and breathe clinical placements. Our team is made up of nurse practitioners, clinical coordinators, placement advisors, and former students who’ve been through the process themselves. We work directly with NP students across the country to help them secure high-quality preceptorships and graduate on time with confidence. - Last updated
January 28, 2026 - Fact-checked by
NPHub Clinical Placement Experts & Student Support Team - Sources and references
- https://nursejournal.org/careers/psychiatric-nurse/how-to-become
- https://nursing.maryville.edu/blog/pmhnp-scope-of-practice
- https://onlinenursing.baylor.edu/news/what-does-psychiatric-nurse-practitioner-do
- https://www.apna.org/about-psychiatric-nursing
- https://www.vhcf.org/demand-for-psychiatric-mental-health-nurse-practitioners-psych-nps-in-virginia/#:~:text=Demand%20for%20Psychiatric%2DMental%20Health,Professional%20Shortage%20Areas%20(MHPAs).
- https://virginiamercury.com/2023/11/08/nurse-practitioners-can-help-increase-virginians-access-to-behavioral-health-care/#:~:text=In%20September%2C%20Centra%20opened%20Virginia's,practitioners%20(PMHNP)%20can%20help.
- https://www.indeed.com/career/psychiatric%20mental-health-nurse-practitioner/salaries/Richmond--VA#:~:text=The%20average%20salary%20for%20a,updated%20January%208%2C%202026).
Find a preceptor who cares with NPHub
Book a rotation.webp)








.webp)


.webp)



%20(3)%20(2).svg)
.webp)