Finding pediatric nurse practitioner preceptors is difficult because of a nationwide shortage of qualified clinicians able to teach. Most pediatric nurse practitioners already manage full patient loads in hospitals and primary care settings, leaving limited time for supervision. Combined with minimal institutional funding, growing NP program enrollments, and fewer available clinical sites, this shortage delays clinical rotations and slows the path to graduation for many NP students.
TL;DR: Why It’s So Hard to Find Pediatric Nurse Practitioner Preceptors
- The U.S. faces a nationwide shortage of pediatric nurse practitioner preceptors, especially in community and non-urban settings.
- Heavy workloads, limited funding, and lack of institutional support make it difficult for clinicians to take on students.
- NP programs continue to grow faster than the number of available clinical sites, creating intense competition among NP students.
- The shortage directly impacts graduate nursing education, leading to delayed graduations and fewer pediatric providers entering the workforce.
- Many students now turn to preceptor matching services like NPHub to connect with qualified preceptors and secure their clinical rotations on time.
Inside the Struggle to Find Pediatric NP Preceptors
For many nurse practitioner students, finding a pediatric nurse practitioner preceptor feels like an uphill climb. You’ve completed the coursework, followed every lead, and sent out countless rotation requests, yet the search for a qualified clinical preceptor still feels endless. What should be an exciting step in your graduate nursing education often turns into a source of stress and uncertainty.
Across nursing programs nationwide, the shortage of pediatric nurse practitioner preceptors is creating delays for NP students who are eager to start their clinical rotations. The number of NP programs has grown rapidly, but the pool of experienced preceptors has not kept pace. Many nurse practitioners already balance full caseloads, charting requirements, and administrative responsibilities, leaving limited time to precept NP students. The result is a competitive environment for clinical placements, particularly in pediatrics, primary care, and behavioral health.
This challenge matters because it doesn’t only affect nursing schools or NP students; it directly impacts children and families who rely on skilled primary care providers. Without enough qualified preceptors, future pediatric nurse practitioners struggle to gain the clinical experience needed to deliver quality care in real-world practice settings.
If your own search for a preceptor has stalled, there’s a smarter way to move forward. Create your free NPHub account to connect with verified pediatric NP preceptors who are actively teaching in real clinical sites. It’s a practical way to find guidance, complete your clinical hours, and stay on track for board certification.
Next, we’ll take a closer look at why this preceptor shortage exists, what’s driving it, and how NP students can navigate it with more confidence.
The Real Reasons Behind the Pediatric NP Preceptor Shortage
One major factor is the closure of pediatric NP programs outside large urban centers. As smaller regional programs shut down, most pediatric clinical education has shifted to major hospitals and children’s medical centers. This means thousands of NP students are now competing for limited clinical sites concentrated in just a few areas. The result is saturation—too many students trying to learn from too few qualified preceptors.
Workload and institutional pressure are also key contributors. Many pediatric nurse practitioners, pediatricians, and primary care providers face demanding patient schedules and rising productivity goals. Even when they want to teach, the time required to precept NP students simply isn’t available. Without financial incentives or protected teaching time, the role of clinical preceptor often falls to the bottom of a long to-do list.
Funding gaps make the situation even more difficult. Unlike adult or family nurse practitioner programs, pediatric-focused training often receives less institutional support. Many hospitals do not offer stipends or recognition for nurse practitioners who take on preceptor roles. In some cases, programs must even limit student admissions because they cannot guarantee enough clinical placements.
Another challenge comes from within the healthcare education system itself. Some pediatricians and advanced practice providers prioritize training medical residents over NP students, reducing access to practicum sites for pediatric-focused programs. With fewer clinical partners available, nursing schools must compete for limited practice settings, leaving students waiting months for confirmation.
All of this creates a ripple effect that extends beyond the classroom. Fewer pediatric nurse practitioner preceptorsmeans fewer opportunities for NP students to develop the clinical skills they need to deliver safe, effective, and compassionate care. It slows the growth of the pediatric NP workforce and limits access to healthcare for children, especially in underserved communities.
Next, we’ll take a look at how the overall pediatric nursing workforce got to this point—and what that means for your clinical training.
The State of the Pediatric Nursing Workforce
To understand why pediatric nurse practitioner preceptors are so hard to find, it helps to look at the broader picture of the pediatric nursing workforce. Data from the Pediatric Nursing Certification Board provides a clear snapshot of where things stand and why demand for clinical preceptors continues to grow faster than the supply.
There are now more than 53,000 certified pediatric nursing professionals in the United States, including pediatric nurse practitioners in both primary and acute care, certified pediatric nurses, and providers with dual certifications. These professionals form the backbone of pediatric healthcare, serving children, adolescents, and young adults in clinical sitesthat range from large hospital systems to community-based primary care settings.
Despite the growth of this field, the distribution of pediatric nurse practitioners is uneven. Many work in major cities or academic medical centers, while underserved areas continue to face shortages of trained pediatric providers. This concentration limits access to clinical placements for NP students outside urban hubs, where qualified preceptors are already stretched thin by heavy caseloads and teaching responsibilities.
The PNCB data also reveals that the pediatric NP workforce is relatively young but highly educated. Most pediatric nurse practitioners hold a master’s or doctoral degree and enter the profession with a strong foundation in nursing practice, clinical education, and child health. Yet, even with this preparation, few go on to serve as nurse practitioner preceptors. Time, workload, and lack of institutional support remain major deterrents, especially in hospital-based practice settings where teaching adds to already full schedules.
This imbalance between growing student interest and limited preceptor capacity has a direct effect on the future of graduate nursing education. Nursing programs want to accept more students to meet national healthcare demand, but many can’t expand without more preceptors and clinical sites to support them.
If you’re starting your own preceptor search, use this knowledge to your advantage. Look beyond hospitals and explore family medicine and community primary care providers who see pediatric patients regularly. And if you want to simplify the process, create your free NPHub account to connect with verified pediatric NP preceptors who are already working with students in real-world practice settings.
Next, we’ll explore how this shortage directly affects NP students and what it means for your path through clinical training.
How the PNP Preceptor Shortage Impacts NP Students
Many nurse practitioner students enter the pediatric track ready for clinical rotations and discover the real obstacle is finding a clinical preceptor who has time to teach. The search stretches on, messages go unanswered, and the timeline for completing required clinical hours starts to slip.
This preceptor shortage disrupts graduate nursing education in practical ways. Limited clinical placements force some nursing programs to stagger start dates or cap enrollment. Students who cannot secure qualified preceptors face delayed graduation, added tuition, and rescheduling with clinical faculty for another term.
Access is uneven across regions. Large cities may have numerous clinical sites, while underserved communities often have few options. Even when students identify potential preceptors, productivity expectations and minimal institutional support make it difficult for busy nurse practitioners to precept NP students.
The impact is more than logistical. Prolonged searches drain energy and confidence during a phase that should build clinical experience and real world skills in pediatric clinical practice. The stress is predictable when timelines are tight and every rotation request feels urgent.
Progress is still possible with a different approach. Start with a focused plan, widen acceptable practice settings, and keep communication short and specific. If you want a structured path, create your free NPHub account to view verified pediatric nurse practitioner preceptors aligned with your program’s requirements. It is a practical way to move from outreach to confirmation and keep your training on schedule.
Ready to take control of the process? Next up is a concise guide to finding your own pediatric NP preceptor, step by step.
A Practical Guide to Finding Your Own Pediatric NP Preceptor
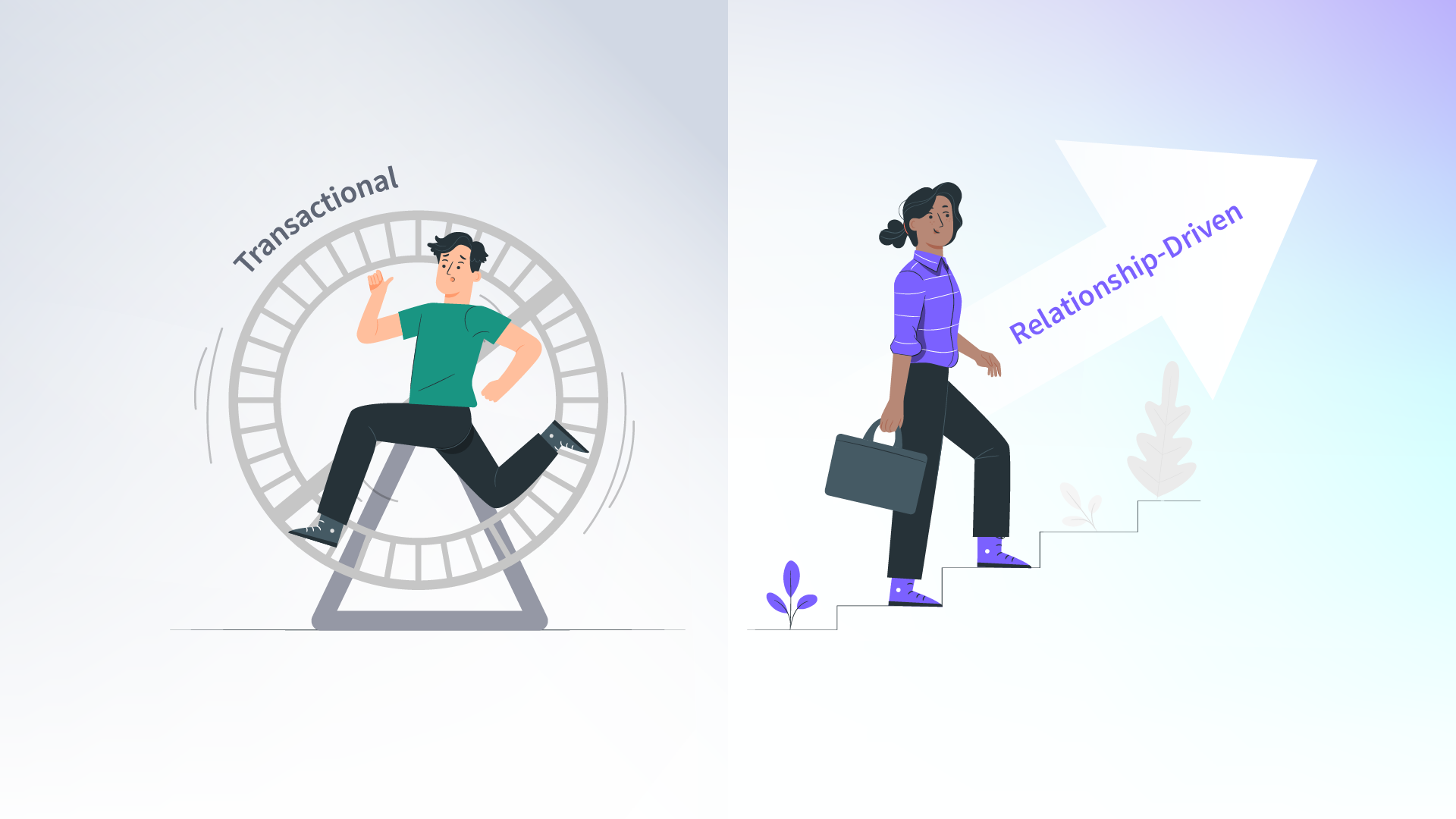
By now, you already know that waiting for the perfect opportunity rarely works. Finding a pediatric nurse practitioner preceptor takes effort, strategy, and patience but with a focused plan, you can make real progress instead of spinning your wheels. These five steps come straight from what’s working for NP students who are successfully securing clinical placements in pediatrics and primary care.
1. Get clear on what your program actually requires
Before you reach out to anyone, review your nursing program guidelines and confirm the essentials: total clinical hours, approved practice settings, and specific preceptor qualifications. When you contact a potential preceptor, include a short, clear summary of what your school expects. It shows you’ve done your homework and saves the preceptor time, which makes them more likely to consider your request.
2. Widen your search beyond traditional sites
Children’s hospitals and pediatric specialty clinics are often full months in advance. Try expanding your search to family medicine, primary care providers, and community health centers that also care for pediatric patients. Many of these sites qualify for pediatric rotations and provide more personalized experiences with smaller patient panels and direct mentoring.
3. Write messages that sound like you
When contacting nurse practitioner preceptors, skip the long formal introductions. A short, personal email that explains who you are, your nursing school, and what kind of clinical experience you’re hoping to gain works best. Mention your interest in pediatrics, behavioral health, or primary care, depending on your program’s focus.
If you’ve already reached out to several clinical preceptors without hearing back, it might be time to try a different approach. Create your free NPHub account to connect with verified pediatric NP preceptors who are currently mentoring nurse practitioner students. You can filter by specialty, location, and availability, which saves time and replaces uncertainty with structure.
4. Use your professional network
Your next opportunity might come from someone you already know. Talk with clinical faculty, classmates, and recent graduates who have completed their clinical rotations. Many are willing to share referrals or introduce you to qualified preceptors they’ve worked with. You can also attend local nursing research events or webinars through the American Association of Nurse Practitioners to meet providers open to precepting.
5. Stay consistent and keep records
Reaching out once or twice isn’t enough. Create a simple spreadsheet to track your contacts, responses, and follow-ups. Consistency shows professionalism and helps you avoid repeating efforts. When a provider does say yes, you’ll already have everything organized to move forward quickly with your clinical faculty and program paperwork.
Finding your own pediatric nurse practitioner preceptor takes time, but every message and conversation moves you closer to your goal. Each “no” brings you closer to the right match, the one who can help you build confidence and develop the hands-on experience you need to succeed in your clinical practice.
If you’re still waiting for your first reply, don’t let the process discourage you. The system may be crowded, but with the right approach and the right support your next step is already within reach.
Next, let’s look at what happens when doing it alone doesn’t work and how NPHub helps students move forward with verified preceptors and real guidance.
When Doing It Alone Isn’t Working
Even the most organized nurse practitioner students reach a point where their own search hits a wall. You’ve emailed every clinical site you can find, followed up with providers, and still haven’t received a clear yes. The longer the silence lasts, the harder it becomes to stay focused on your clinical education instead of the stress of waiting.
That’s where using structured preceptor matching services can help. Instead of starting from scratch with every rotation, you gain access to a network of verified pediatric nurse practitioner preceptors who are already teaching students in approved practice settings. This approach takes the uncertainty out of the process and gives you a direct path toward completing your clinical hours and finishing your NP program on time.
With NPHub, everything begins with clarity. Each nurse practitioner preceptor in the network is reviewed for preceptor qualifications, active licensure, and experience in pediatrics, primary care, or acute care. You can view available clinical preceptors, learn about their practice setting, and choose opportunities that align with your program’s requirements before you reach out.
The process is simple:
- Verified professionals who meet national standards for graduate nursing education
- Clear communication between students, schools, and clinical faculty
- Support with coordination and paperwork so your rotation starts smoothly
- Real human guidance from the NPHub team to help you stay organized and confident
When you’re balancing coursework, exams, and a full-time job, finding your own pediatric NP preceptor can start to feel impossible. Using NPHub doesn’t replace your effort, it builds on it. You bring your goals, and the platform helps connect you with experienced preceptors who can make those goals possible.
Moving Forward, One Rotation at a Time
You’ve made it through the toughest part of the process: not just studying, not just showing up, but refusing to give up when everything around you said it would be easier to wait. That kind of persistence is what sets great pediatric nurse practitioners apart from the rest.
The preceptor shortage is real, and it’s not something any single student can fix. But you can still move forward, one message, one connection, one rotation at a time. Every hour of hands-on experience, every child you assist, every skill you build gets you closer to the provider you’re becoming.
And you don’t have to do it alone. Create your free NPHub account, connect with verified pediatric nurse practitioner preceptors, and take the next real step toward completing your clinical rotations and earning your certification.
Because the world doesn’t just need more NPs, it needs the kind of providers who’ve learned how to keep going even when the path gets hard. That’s you. And you’re closer than you think.
Frequently Asked Questions About Pediatric NP Preceptors
1. Why is it so difficult to find Pediatric Nurse Practitioner preceptors?
The current preceptor shortage is caused by several overlapping issues. Many pediatric nurse practitioners balance demanding clinical practice schedules, while others face limited institutional support to teach NP students. At the same time, the number of nursing programs continues to grow, increasing competition for available clinical sites. These factors make it challenging for nurse practitioner students to find qualified preceptors on time.
2. What qualifications should a Pediatric NP preceptor have?
A nurse practitioner preceptor must hold an active license, meet your program’s requirements, and have sufficient clinical experience in pediatrics, family medicine, or another relevant specialty. Some nursing schools may also require national board certification from the Pediatric Nursing Certification Board or equivalent organizations. Always confirm with your clinical faculty before starting your clinical rotation.
3. What is the role of a Pediatric Nurse Practitioner preceptor?
A pediatric nurse practitioner preceptor is typically an experienced pediatric NP, nurse practitioner, or qualified healthcare professional with expertise in caring for children and adolescents. Depending on your nursing program’s requirements, some primary care providers or pediatric clinicians in community health or acute care settings may also qualify to precept NP students. The most important factors are active licensure, relevant clinical experience, and a willingness to guide students through hands-on clinical education in pediatrics.
4. What types of clinical sites qualify for Pediatric NP rotations?
Approved clinical sites vary by program but often include primary care clinics, community health centers, urgent care facilities, and pediatric outpatient practices. Some clinical placements may also occur in behavioral health or women’s health settings that provide pediatric services. The goal is to gain hands-on experience with diverse patients and practice environments that reflect real-world nursing practice.
5. How early should I start my preceptor search?
Ideally start six months before your clinical rotation begins. NP preceptors often schedule their students far in advance, and popular practicum sites fill up quickly. Early planning gives you more time to find the right preceptor and complete all necessary documentation with your school and clinical faculty.
6. What should I include when I contact a potential preceptor?
Keep your message brief and professional. Include your name, nursing school, NP program, total clinical hours needed, and preferred practice settings. Mention your learning goals and any specific specialties or patient populations you hope to work with. Clarity helps the prospective preceptor decide quickly if they can meet your needs.
7. How can I improve my chances of finding a preceptor?
Use your professional network—talk with instructors, classmates, and alumni who may know experienced preceptors in your area. Attend local nursing research or continuing education events to connect with healthcare professionals who enjoy teaching. If you still need help, use preceptor matching services like NPHub to connect with verified pediatric nurse practitioner preceptors available for your upcoming rotation.
8. What happens if my preceptor cancels last minute?
Contact your clinical faculty immediately. Most nursing schools can help locate another clinical site or temporary placement so you can continue your clinical education without major disruption. Services like NPHub can also help you find a replacement preceptor quickly to prevent delayed graduation.
9. How do preceptor matching services actually work?
Platforms such as NPHub simplify the process of finding nurse practitioner preceptors by connecting students with vetted professionals who meet preceptor qualifications and program requirements. These services manage the coordination, paperwork, and communication between students, schools, and preceptors, allowing you to focus on learning and completing your clinical hours.
10. How do I get started with NPHub?
You can create your free NPHub account to view available pediatric nurse practitioner preceptors across multiple practice settings. Once you find a suitable match, NPHub assists with scheduling, documentation, and confirmation, helping you secure your clinical placement and complete your NP program on time.
Key Definitions
- Pediatric Nurse Practitioner (PNP):
An advanced practice nurse practitioner specializing in the healthcare of infants, children, and adolescents. Pediatric nurse practitioners diagnose and manage acute and chronic conditions, perform physical assessments, prescribe medications, and promote health education and disease prevention in both primary care and acute care settings. - Clinical Rotation:
A structured, supervised clinical experience where nurse practitioner students practice under a licensed provider in an approved clinical site. Clinical rotations are an essential part of every NP program, allowing students to build clinical reasoning, communication, and patient management skills across multiple practice settings. - Clinical Placement:
The process of assigning NP students to clinical sites or practicum sites that meet their program’s requirements. Successful clinical placements depend on collaboration among nursing programs, clinical faculty, and preceptors to ensure each student meets academic and professional competencies. - Preceptor Matching Services:
Professional matching services that connect nurse practitioner students with qualified preceptors who meet specific preceptor qualifications. Platforms such as NPHub streamline the process by verifying licensure, coordinating paperwork, and helping students secure clinical placements that align with their nursing program and certificationgoals. - Clinical Faculty:
Educators within nursing schools who oversee clinical education, evaluate student progress, and ensure compliance with institutional and accreditation standards. Clinical faculty act as liaisons between preceptors, students, and nursing programs to support high-quality graduate education and professional development.
About the author
- NPHub Staff
At NPHub, we live and breathe clinical placements. Our team is made up of nurse practitioners, clinical coordinators, placement advisors, and former students who’ve been through the process themselves. We work directly with NP students across the country to help them secure high-quality preceptorships and graduate on time with confidence. - Last updated
October 28, 2025 - Fact-checked by
NPHub Clinical Placement Experts & Student Support Team - Sources and references
- https://www.pncb.org/sites/default/files/resources/PNCB_2022_Pediatric_Nursing_Workforce_Demographic_Report.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10606953/pdf/nihms-1929654.pdf
- https://www.nphub.com/rotation-paperwork-process
- https://www.nphub.com/preceptor-matching-specialists
- https://www.nphub.com/np-student-coordinators
Find a preceptor who cares with NPHub
Book a rotation.webp)








.webp)

.webp)



%20(3)%20(2).svg)
.webp)